NHS 70: What lessons for Wales from around the UK?
- Published

What could the health service in Wales learn from the other UK nations? What problems do we share - and how could we do things differently? I went on a journey to find out.


LESSONS FROM NORTHERN IRELAND
How is it different?
Since 1972 it has an integrated system for health and social care - a "one stop shop" - although some critics say the NHS still dominates and social care has been a "poor relation".
What is it good at?
The legacy of the troubles has had an impact, leading to high rates of mental health problems. But there are innovative solutions, especially in the community and taking care out of hospital.

Resident Tommy Cuthbert feeding chickens at the supported living community he lives at
We saw a small estate for people with mental health issues, living in their own rented homes with gardens, built next to the site of an old asylum. The 26 people all have individually-focused plans with support from housing, health and care workers as they need it. I spoke to one of the residents Tommy Cuthbert, who said he had "more confidence" and was "happier".
But what are the problems?
Prof Deirdre Heenan, social policy expert at Ulster University, said Northern Ireland's experience showed that just combining health and social care structures is not enough and you also need "cultural integration" so people think and work together. Waiting times, vacancies and health outcomes are also big issues, not helped by a political vacuum.
"We're in a no man's land... with no one in charge," said Prof Heenan. "Decisions aren't being made, we have no health minister, no health budget - no agreement on a strategic vision. We've reverted to keeping the show on the road."
What could NHS Wales learn?
A small population and integrated system on their own are not enough. But where different areas work better together, it can make a difference.
A shared vision for mental health services in the community, backed up by evidence that it works, is "a no brainer," according to Peter McBride, chief executive of Inspire social care provider.
"The NHS is a big institution - the big challenge is how it changes, the only rational and legitimate argument is that it will benefit patients. We must show there are better ways of getting outcomes, more efficient and more economic," he said.


LESSONS FROM SCOTLAND
How is it different?
It has long been considered to be the best performing in terms of waiting lists - including for referral to treatment times and in A&E. This is despite having similar challenges to Wales in terms of balancing the needs of a widespread rural areas and dense urban centres with challenges of deprivation.
Its continuity of approach to improving quality has been highlighted as a strength too.
What is it good at?

Eddie Solberg is able to get help from his physiotherapist Linda via an iPad session for help with his stroke recovery
Innovation. One example I saw was how even a physiotherapy appointment could happen through a smart phone link with a stroke patient in his home. But it's not just imposing new gizmos and gadgets but actually listening to what patients want. Ways of working which save them time.
Health professionals here want to look beyond the numbers to the quality of life for patients too.
But what are the problems?
Despite its record, there has been a recent deterioration in performance. and controversies over mental health.
It still faces challenges from tackling inequalities in people's health and in common with other UK nations has financial pressures.
And there is a demand for political impetus to drive change - including seamless care in the community.

You might want to read these stories too:

Prof George Crooks, chief executive of the Digital Health and Care Institute, said: "It's the same as everywhere - we need brave leadership, brave and difficult decisions that are followed through on and a conversation that everyone can understand and have their say. For me, we're getting better at that."
What could NHS Wales learn?
Scotland after devolution has arguably had more confidence to do its own thing rather than looking over its shoulder at what England is doing.
It is further down the line in using legislation and other initiatives to get health and social care working together.


LESSONS FROM ENGLAND
How is it different?
Size is obvious - NHS England is 15 times bigger than its Welsh counterpart and employs 1.3 million people, one of the world's biggest organisations. But it is also more complex. There is an internal marketplace and it means more competition and choice as to where a patient gets treated.

An image from a hybrid scanner, which does the work of two at once, with radiologist Lubna Hussain
What is it good at?
Helen Buckingham, strategy director at Nuffield Trust, believes looking back there have been improvements on targets. "When I first started purchasing health services as a young finance person, the maximum waiting time for inpatient care was two years," she said. "Now it's 18 weeks - a real improvement.
"There was more money put into the system but we also had a root and branch look at how services were delivered. We can still look at improvements but it is getting harder - and none of us are convinced that just telling people to work harder is going to be the answer. Now we need to help people get under the skin of what the issues are."
England also has some of the biggest and best known teaching hospitals in the world - and is involved in world-leading medical and pharmaceutical research.
Radiologist Lubna Hussain showed me a £1m hybrid scanner at Hillingdon Hospital in Uxbridge. It sounds like a lot of money - and it is - but it cuts down on the number of times a patient has to visit because it gives you two different sets of information at once.
The technology and imaging is also cutting edge.
"Now there's far more accuracy determining where the problem is," said Ms Hussain.
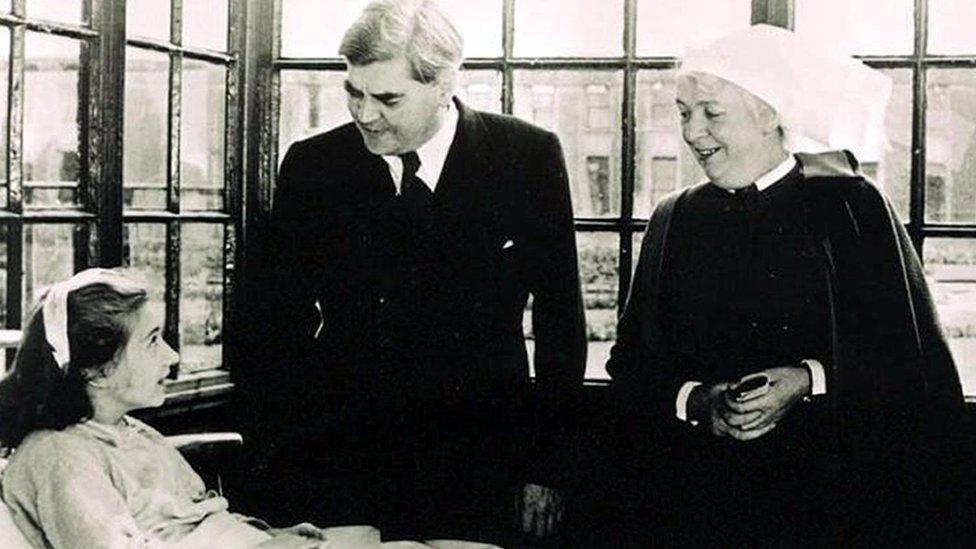
Helen Buckingham, Prof George Crooks and Prof Deirdre Heenan with views from England, Scotland and Northern Ireland
But what are the problems?
Its sheer size. There are great ideas in some areas - but how do you shift those around the country?
There is the commissioner-provider split - the relationship between purchasers holding the budgets and the hospitals and trusts doing the work. Is this effective? One expert told me competition can be really useful in offering a range of providers for patients - but this might not work quite so well for very specialist services.
Budget squeezes on local authorities have had an impact on social care, which is seen as better protected in Wales.
What could NHS Wales learn?
The NHS - a 'political football' in the UK
The approach in England has been described as an approach of "targets and terror" where it is not unheard of for ministers to admonish individual NHS chief executives if they fail to deliver.
Some argue this firm hand is effective although Welsh Government has preferred to take more of a partnership approach.
However, a report by independent experts the OECD said Wales needed to employ a stronger "guiding hand" and exert more central control to get things done.
There are signs this may be starting to happen now. We've already seen our health secretary offering financial incentives to cut waiting times - and withholding money when targets are not met. Meanwhile, a new NHS Wales "executive function" will sit above health boards to help speed the process of making big decisions about hospital services in the future.
Jennifer Dickson, chief executive of the Health Foundation said no one system in the UK was superior to the other.
"There's more variation within England than across the four nations," she said.
"We have quite a lot to learn from each other at local level. What's striking at a national level is how similar our performance is - despite the political differences in how the system is shaped."
- Published3 July 2018

- Published2 July 2018

- Published1 July 2018

- Published2 July 2018