Betsi Cadwaladar's three-year plan to stop failures
- Published

The boss of north Wales' health board has said a three-year transformation plan is essential to stop it "underperforming and overspending".
Under-fire Betsi Cadwaladr - which has been in special measures for nearly four years - has been criticised for the absence of a long-term strategy.
It says its set-up is "inefficient, unaffordable and not sustainable".
The plan focuses on more specialist hospital care as well as boosting community support for GPs.
Betsi's new chairman Mark Polin, the former chief constable of North Wales Police, believes a "fundamental shift" is required.
"The bottom line is that status quo is not an option," he said.
"We're underperforming and overspending against the allocation by Welsh Government - and those two things cannot continue. We've got to be clear about how we deliver services going forward and change, in my view, will be necessary."
He said health services could be in jeopardy "unless we get our act together."

Mark Polin took over last September and spent a few months before looking at the organisation
Mr Polin has been in post since last autumn and said a clear sense of direction needed to be in place and the board needed to deliver on promises if it was to improve.
It is nearly six years since a damning report into the way the health board was run, including a failure to plan ahead for big changes.
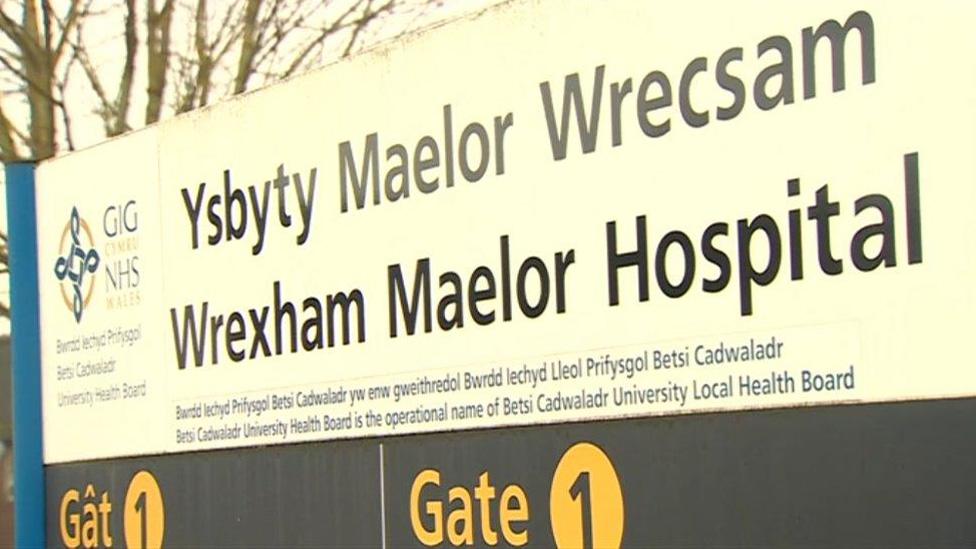
But as well as problems with mental health services, in more recent months, two of its three hospitals have posted the worst A&E waiting times on record in Wales.
The health minister has also been frustrated at the rate of progress, calling its worsening financial position "disheartening and unacceptable".
He said on Tuesday that Betsi would remain in special measures because, despite improvements, it still faced challenges.
What are Betsi's challenges?
It is struggling with waiting times, particularly at A&E at Glan Clwyd and Wrexham Maelor hospitals, while waits for operations such as replacement knees and hips or eye surgery are also too long - way above the Wales average
Growing difficulties in attracting new GPs and staff shortages in a number of specialisms, while spending on agency nurses to cover rotas is as high as £1m a month
Financial challenges - the budget deficit could be as high as £42m by the end of March, more than last year
Bed occupancy rate in hospitals is currently over 90% - this risks bed shortages, periodic bed crises and increased infections
Size and condition of its 130 health buildings - too many are older, inefficient or unsafe.
This new arrival is being looked after at the £18m neonatal unit at Glan Clwyd

Work on the new community hospital in Rhyl is expected to start next year
What is already happening?
A new £40m North Denbighshire community hospital is planned for the site of the Royal Alexandra Hospital in Rhyl by the end of 2022.
There is also an £18m Neonatal Intensive Care Service (SuRNICC) at Ysbyty Glan Clwyd, which means some babies who may have had to travel to England for treatment can now stay in north Wales.
Major vascular and arterial surgery will be centralised at Glan Clwyd from April - rather than trying to doing these operations in three hospitals. Eight specialist consultants will work together and also cover on-call.
Dr Emma Hosking, hospital medical director, said they had already recruited six consultants.
"The rotas on all three sites were becoming more onerous because we only had two or three doctors in each place, trying to be all things to all patients and that meant as soon as anyone was away or was ill, it became very difficult and the service became fragile.
"Since it's become very clear this is happening, we've found it increasingly easy to recruit. We've also been encouraging to the recruiting to the nursing posts."
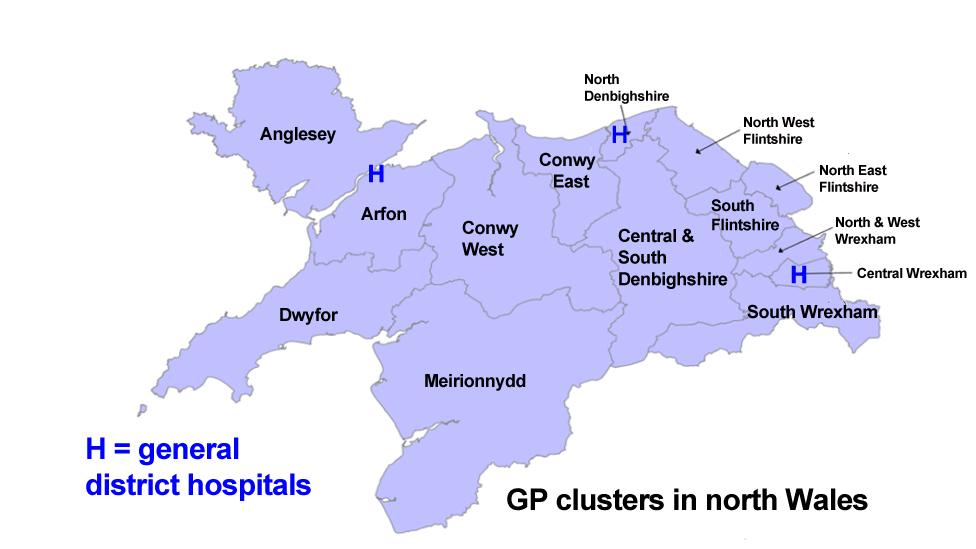
Community health teams would be built up in the existing 14 GP clusters
What might it look like?
The three-year plan would see A&E, consultant-led maternity and paediatric services continuing at all three district general hospitals - Bangor, Glan Clwyd and Wrexham Maelor
While patients might need to be transferred to hospitals for more specialist care, it hopes to widen the range of specialisms so people will have to travel outside the area less frequently
Inpatient urology, acute stroke and orthopaedic surgery done at fewer hospitals, while developing a pelvic cancer centre with robot-assisted surgery
Major physical trauma injuries, neurosurgery, specialist treatment for children and some cancer treatments will still be outside north Wale, but the health board wants to make testing and diagnosis "as local as possible"
Developing 14 existing GP clusters in north Wales by building up the community health teams - with a training academy to boost nursing, therapy, pharmacy and mental health to help support GPs and reduce their workload
After a major refurbishment of Glan Clwyd Hospital, Wrexham Maelor could also be the next to be tackled.
Plaid Cymru has called for any changes to consider the rural nature of north west Wales.
"So far, we have seen services moving eastwards but the board must consider travel problems and distances between different centres across the north west before making substantial changes," said a spokesman.
Mr Polin said despite the difficulties there had been improvements, including in GP out-of-hours and mental health services.
But the health board was going to have to "hold our nerve," be involved in some difficult conversations but stick with the plan. It has been published in a draft form and with a detailed timeline expected by September.
"If I was Welsh Government, I wouldn't be taking this organisation out of special measures because some of the fundamentals are not in place," he added.
"That's not a criticism, it's a fact. If we can demonstrate that there's a higher level of leadership, that direction is clear, governance is tight, the staff feel supported and engaged, and we have the infrastructure in place, then I've every expectation we'll move out of special measures."
- Published20 September 2018
- Published5 June 2018
- Published11 May 2017

- Published20 September 2016

- Published8 June 2015

- Published27 June 2013
