Coronavirus: Newport intensive care doctors prepare for surge
- Published
Consultants are being asked to prepare to treat 10 times the normal numbers of intensive care patients, if there is a surge in coronavirus cases.
Dr Ami Jones is looking after 13 patients on ventilators at Nevill Hall Hospital in Abergavenny, Monmouthshire, which is double the usual number.
Staff at Newport's Royal Gwent Hospital are preparing to expand services more.
"If we have to get to that 10 times capacity surge, we're going to be absolutely at the limit," she said.

Royal Gwent Hospital in Newport and Nevill Hall its sister hospital are preparing to expand intensive care
Dr Jones, who works between the two hospitals, said: "We're seeing huge numbers of sick patients needing ventilatory support.
"The patients are quite young, quite fit and well. Some of the younger patients are in their 20s, the older ones in their 70s. And they've all got the same thing - inflamed lungs, all needing significant amounts of help on ventilators.
"There is an element of 'wow, that could be me, but for the grace of God'."
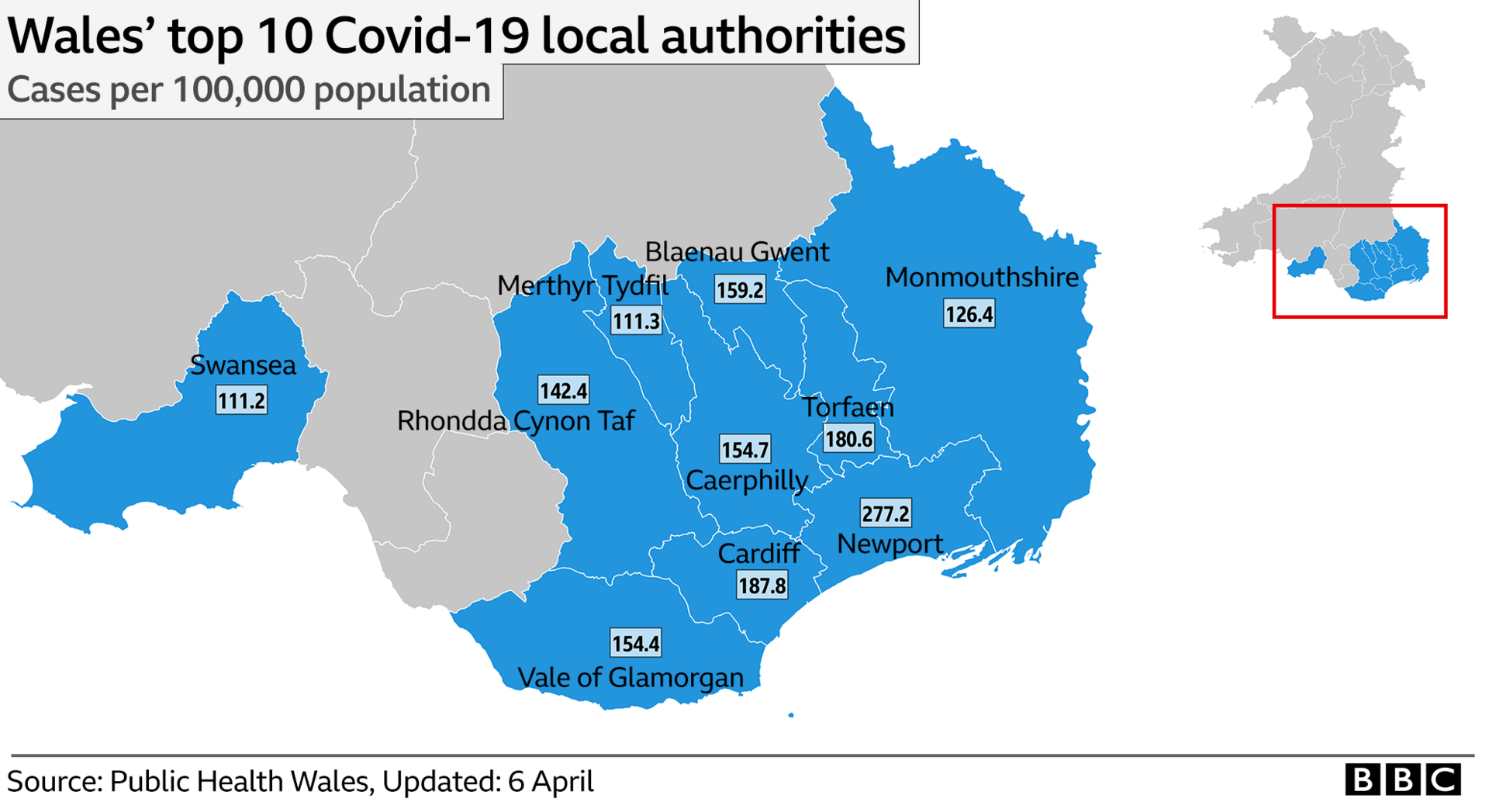
Where are most cases of coronavirus?
More detailed data from Public Health Wales published on Monday, external shows Newport is the hotspot for positive tests.
It has had more than 277 cases per 100,000 of its resident population - 425 so far.
This follows concern in recent weeks that Aneurin Bevan health board had become a hotspot, although NHS officials say the caseload appears to be moving from east to west.
Newport's rate is far higher than the proportion anywhere else - Cardiff, which is second, has 187.8 cases per 100,000.
The lowest is Conwy county, with 19.6 cases per 100,000.


Dr Ami Jones said she had young people in her intensive care unit who might die
Dr Jones said intensive care staff were facing challenges from the "sheer numbers" coming in with low oxygen levels.
Despite the use of video to link with families, she said staff also had to be there to offer emotional support for patients, because they could not risk relatives being there.
Dr Jones said she had what she needed as things stood, with her intensive care unit expanding to two wards, with more ventilators starting to turn up.
"We could probably increase our capacity by four times, but we've been asked to potentially go up to 10 times our capacity," she said.
"If we have to get to that 10-times capacity surge, we'll going to be absolutely at the limit.
"If we go beyond that, I don't know what happens after that - that's what people are talking about running out of ventilators and space in hospitals."
Dr Jones also said while people were "not going to get one-to-one nursing care from an intensive care nurse, they'll end up being looked after by someone else - very well, I'd hope".
- Published31 March 2020

- Published11 March 2020

- Published4 May 2020
