Covid: Doctor 'has shed more tears than ever'
- Published
Dr Bethan Gibson is hoping for some kind of normality by Easter
A senior intensive care doctor says she has shed more tears during the pandemic than in her entire career as staff struggle to cope with demand.
Dr Bethan Gibson, from the Royal Glamorgan Hospital, said the Christmas lockdown was "vital" amid rising critical care numbers.
She said the pandemic had been "relentless" on staff, with many taking time off with burnout or stress.
But she hopes vaccination is a signal for some kind of "normality" by Easter.
The hospital, in Llantrisant, is one of the general hospitals in the Cwm Taf Morgannwg health board, which has recorded the most coronavirus-related deaths (949) in Wales.
Dr Gibson said the scale of the problem has taken a toll on staff.
"I don't think anyone can really appreciate what it's like to be an ITU nurse in particular at this current time," she said.
"They've got the pressures of more work because there's more patients.
"They're looking after maybe double what they normally would, or having to support nurses who are maybe not familiar with the unit. They're in PPE for hours on end."
Shortages of staff is more problematic than a shortage of beds, with many staff forced to take time off for shielding, isolation, burnout or post-traumatic stress.
"There's no point having a bed and a ventilator without a nurse and some medical professionals to help with looking after that patient, and that's what we're really struggling with, our staffing," she said.
Dr Gibson added Covid-19 has changed the way intensive care staff have interacted with patients, who are generally conscious on the ward despite being very sick.
Medical staff are seeing the "fear in the eyes" of patients who are conscious, but being told they may not survive the illness.
"That's one bit I've personally struggled with," she said.
"Usually if they're really sick and need intensive care, they're barely conscious.
"With Covid... their numbers are really, really sick, they're hypoxic, you're scared they're going to arrest and yet they're fully awake, they're not really in distress, they're able to talk to you.
"But they are now acutely aware of how sick there are, they're begging and pleading with us to make sure they don't die."
Covid patients speak of their frightening experiences at people not following lockdown rules
She added more than half of Covid patients on intensive care die, compared to about a fifth of patients before the pandemic.
Wales brought forward its level four national lockdown by eight days to start on 20 December, a decision welcomed by Dr Gibson as "vital" for hospitals struggling to cope with the rise in admissions.
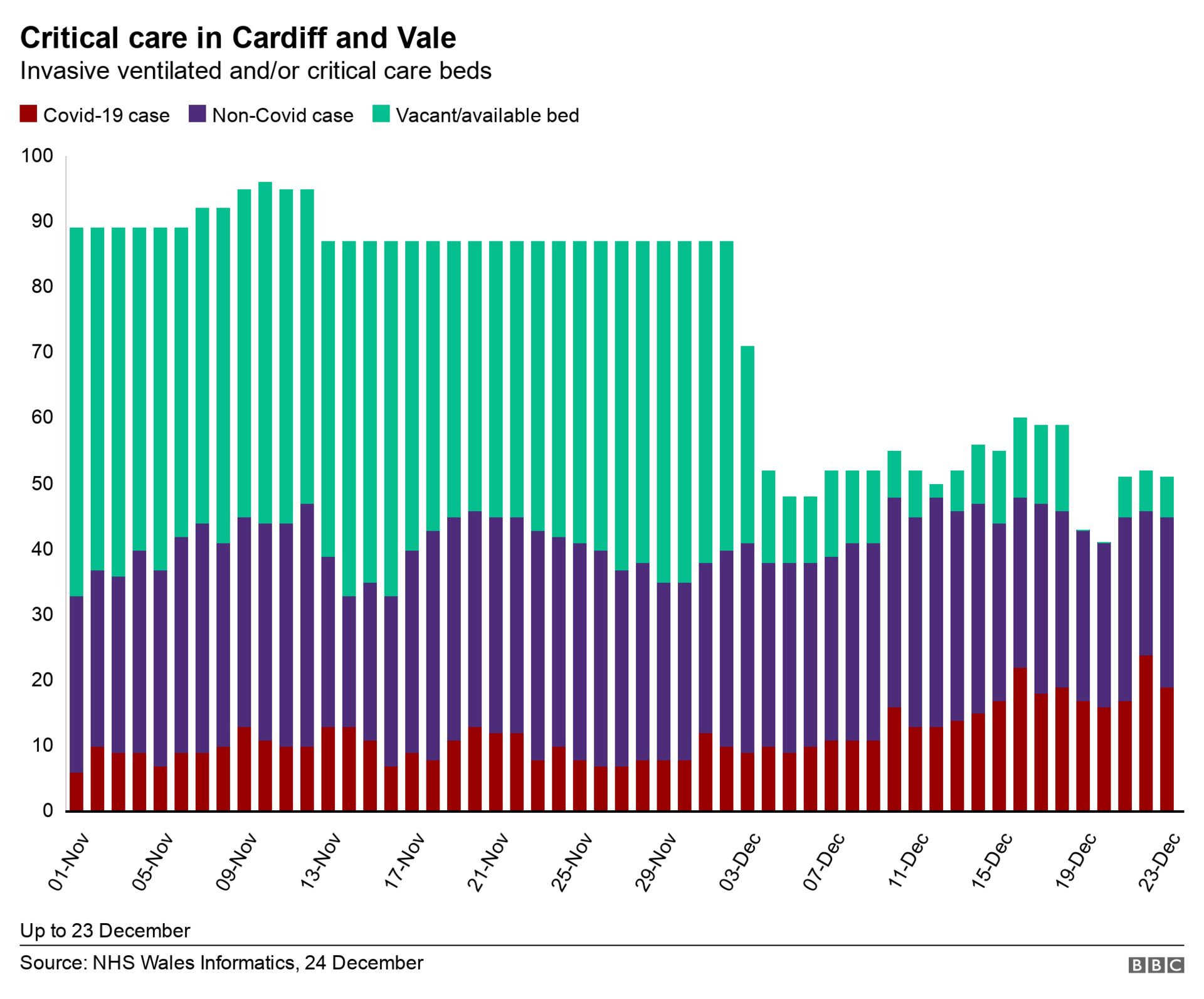
"It's going to hopefully get us to a plateau stage where we can cope with the numbers that we currently have and hopefully the numbers coming in with Covid will drop significantly in the next few weeks."

NHS staff are spending long periods in full PPE
While the so-called second wave of cases has felt "relentless" for medical staff, Dr Gibson sees the start of vaccinations in Wales as a light at the end of a long tunnel.
"We have to have some goal and some light otherwise it would be even harder," she said.
"We're learning all the time how to manage patients with Covid and that's a positive.
"The testing is also paramount and that's improving. I'm hoping by Easter we might be able to return to some normality."
- Published27 December 2020

- Published22 December 2020

- Published9 December 2020

- Published2 December 2020

- Published10 November 2020
