Covid: NHS Wales hospital waiting list hits record 538,861
- Published

Nearly two thirds of orthopaedic patients face a wait above 36 weeks.
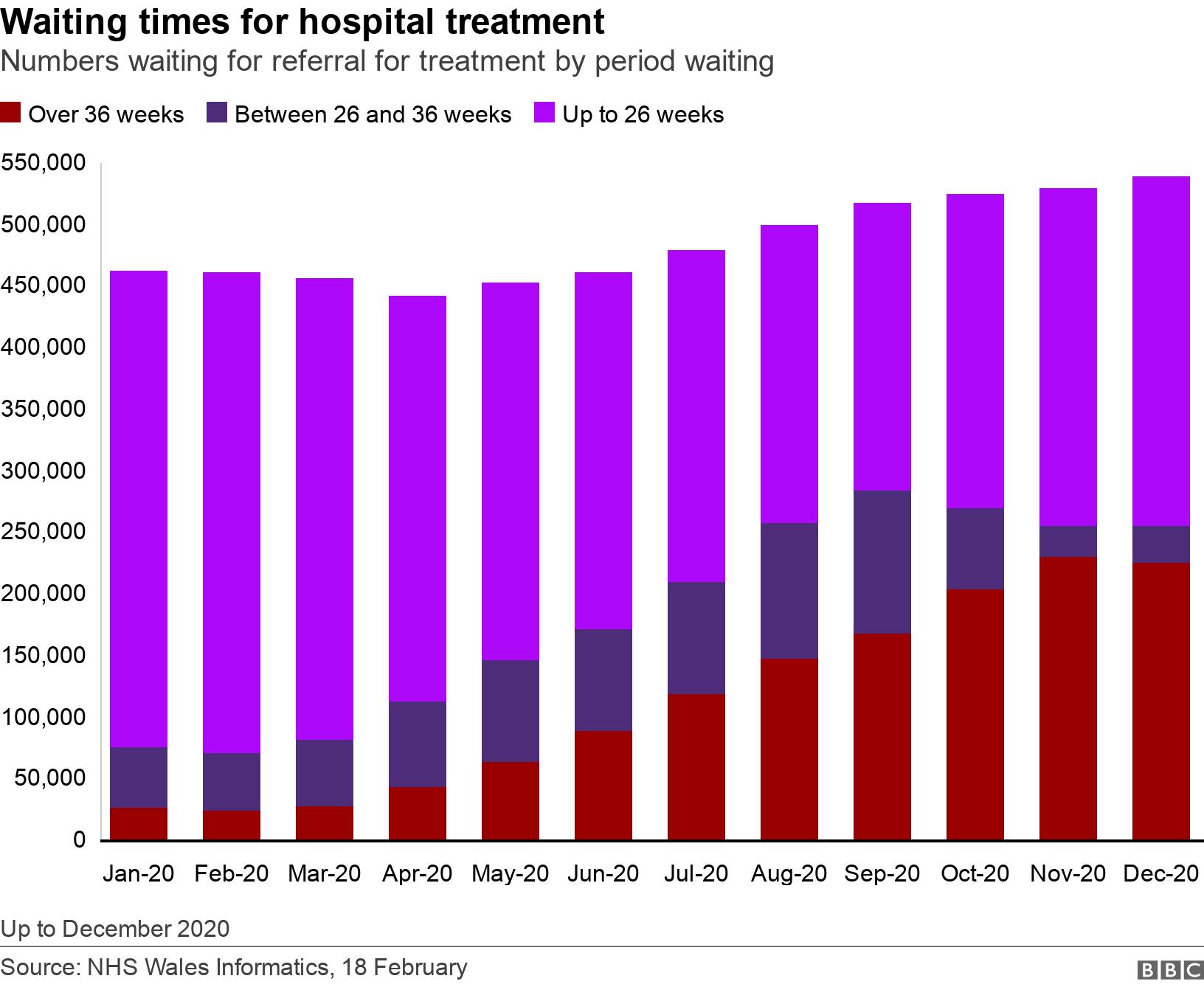
Numbers in Wales who are waiting for non-urgent hospital treatment have hit a record high of 538,861.
More than 82,000 people have been added to the list since last March, latest NHS Wales figures show.
It comes after the number of those waiting more than nine months grew by eight times to 226,138 people, from 27,314 in January 2020.
In-roads have been made on the longest waits, with nearly 5,000 fewer on the list in December than the month before.
Waiting lists grew after most non-urgent treatment was postponed in March to prepare the NHS for Covid patients.
But the NHS has been trying to continue with surgery in recent months, although continuing pressure has forced some postponements.
Chris Jones, deputy chief medical officer for Wales, said it would be a "mammoth task" to clear the backlog.
He said: "The backlog for some categories of patients has increased because it's still difficult, even though the number of people in our hospital with Covid has decreased.
"We still [have] around 2,000 people with Covid-related problems in Welsh hospitals and of course those people would not have been there a year ago, so that is a big challenge but we do need to start getting other care, other services, online as quickly as possible.
"We don't have backlogs for cancer care [but] there are other huge backlogs for surgery, orthopaedic surgery, other types of surgery, endoscopy procedures… and these have to be cleared but it will be a mammoth task and it will take a considerable period of time."
The Welsh NHS Confederation said in a statement the figures showed the "scale" of the task facing the health service.
It added: "We know this is hard for people... but there is some hope on the horizon and the NHS will do all it can to deal with that backlog once we come through the pandemic."
How many people are now waiting?
We can now see all the figures for 2020 and they show:
The overall waiting list for treatment is a record 538,861
Numbers of patients waiting more than 36 weeks - nine months - to start treatment in hospital have grown from 27,314 in January 2020 to 226,138 (an increase of 728%)
In-roads have been made into those longest waits in the last month - the number of patients fell by 4,884
The longest waits included 52,100 people due for orthopaedic or trauma treatment - a near 500% increase since January 2020 - and 254 waiting for cardiothoracic surgery, nearly six times as many
Another 1,515 are waiting for neurological treatment - compared to 28 at the start of the year. These specialities have seen some improvements over the latest month
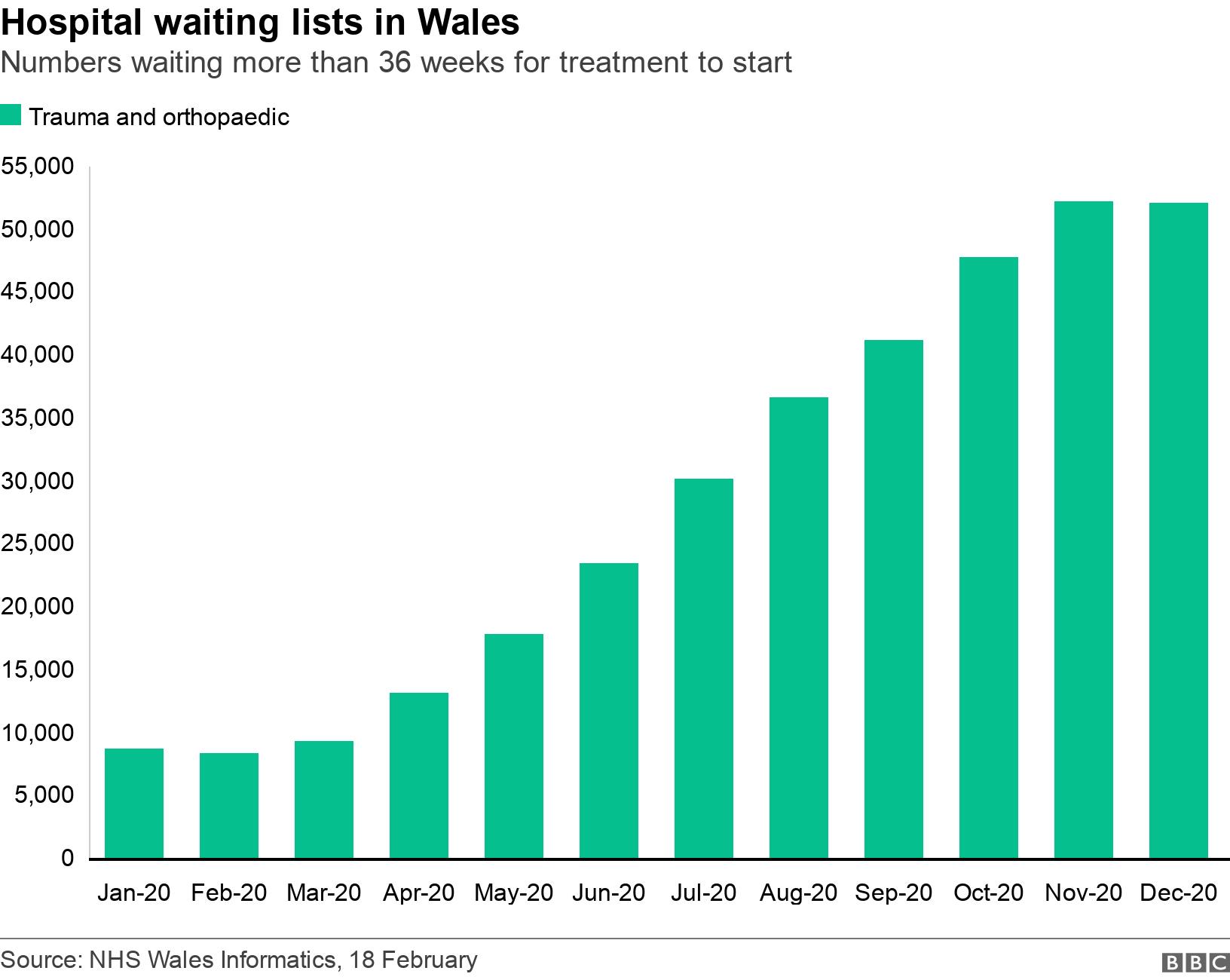
Orthopaedics bear brunt
But the likes of hip and knee operations are where the numbers waiting the longest are the greatest.
There are more than 80,340 people waiting for treatment to start.
Nearly two thirds face a wait above 36 weeks.
The overall list meanwhile has risen by nearly a quarter since January.
Welsh Government targets state 95% of patients should be treated within six months and nobody should wait longer than six months.
Experimental performance measures, January 2021
44,500patients seen across A&E units
16minutes average wait, time to triage
64minutes average wait, time to see clinician
43.7%no follow-up required
27.15%patient admitted to hospital
New measures for A&E performance
Along with waiting times figures, the Welsh Government is now publishing, external three new "experimental" performance measures for A&E departments, for January:
Time to triage: This is the average time someone has to wait for an initial assessment - and performance by triage category (how urgent your condition appears to be) is broken down into three categories - immediate, very urgent and urgent. Those very urgent or urgent had 15 and 17 minute median waits. This is a minute quicker than the month before
Time to clinician: The average time a patient waits for a more thorough assessment by a clinician - 63.1% were said to be seen within a "valid time" - and the median time was 64 minutes
Outcome: Information on where people end up after being assessed and treated at the emergency department. It shows among other outcomes that 27.15% were admitted, 43.7% needed no follow-up, while 11.4% were referred to a GP
No targets have been set in relation to these measures and the Welsh Government said they were set with input from front-line emergency care staff.
The current target is 95% of patients should spend no longer than four hours in A&E, but this has never been met since it was introduced in 2010.
The waiting times for A&E in January showed 74.2% of patients were seen, transferred or discharged within four hours, a 4.2% improvement on December.
The worst performance was only 42% seen within four hours at Glan Clwyd hospital.
There were 5,462 patients across Wales who waited more than 12 hours, even though the targets state nobody should have to wait that long. This is 924 fewer patients than the month before.
Other figures show:
There were an average of 2,530 referrals for first outpatient appointments a day in December, 19.2% down on the year before
11,717 cancer patients started on the treatment pathway in November - 9.3% fewer than the year before but NHS Wales said numbers were at a "broadly similar level" to pre-Covid numbers
65.6% of newly-diagnosed cancer patients began treatment within 62 days from the point of suspicion on the single cancer pathway. This is 2.4% higher than a year ago
For the ambulance service, 59.6% of emergency responses to immediately life threatening (red) calls arrived within eight minutes. This is the sixth month in a row that the 65% target has not been reached. Covid protocols, including extra PPE impacts on the speed at which they can respond to a call

'There are times when I don't cope, I know I'm not the only person like that'

Lorraine Ledwell, left, has been waiting for a hip operation for almost two years
Teaching assistant Lorraine Ledwell has been waiting for a hip operation for almost two years.
She tries to cope but her arthritis causes her constant pain.
The 53-year-old does not sleep well because she gets up every few hours to take painkillers.
She says she cannot do much on weekends as she spends the time catching up on sleep.
"I don't want to be that person that takes tablets every (few) hours, that can't sleep because of pain," she said.
"I don't want to be that person. I want to be the person that I was, that could sit on the floor with my children at work.
"I can't do that anymore.
"I'm still a good auntie and great auntie, but I want to be that one who can sit on the floor and really play with the little ones."
She says she misses being active.
"I want to be that person again without hurting."
Her condition causes her to suffer a constant dull ache.
When she walks pain "radiates" down her leg.
"At the moment there are times when I don't cope, and I know I'm not the only person that is like that," she said.
So far Lorraine, from Bridgend, has been on the waiting list for 97 weeks.
"When I went for the initial referral they said it would be about a year," she said.
"I knew the waiting list was going to be that time, it's just a given."
Having once worked for the NHS she knew it was busy.
Now she just wants to get back to "normality."
She said: "Physically I can cope to a certain point, there are certain strategies, certain things I can do to help with the physical pain day to day.
"I find it is tougher mentally because I am waiting for a call. Every time I hear a phone ring or see a number I don't recognise I think, 'That is them calling.'
"That is the point where they are going to say 'Right, your journey is starting.'
"I want to start my journey.
"I thought I had started it two years ago and nothing happened, it completely stalled.
"It seems funny to say that I want to go through that pain, that I want to go through having parts of my bone removed.
"But I want to go through that because I know that, at the end of that journey I am going to be a happier person, because I'm not in pain."


- Published21 January 2021

- Published28 May 2024
- Published23 December 2020
