Brecon woman 'dependent' on drugs prescribed to treat her
- Published
Niki Jones had two horses and a successful career before she developed chronic pain
A woman with chronic pain says she is "dependent" on the medication prescribed to treat her.
Niki Jones has spent more than 18 years on various high-strength drugs to treat pain she began experiencing aged 31.
The 49-year-old from Brecon said they made her worse and she only started to recover using other treatments.
New guidance says people with chronic primary pain should not be started on drugs but recommends exercise and psychological therapies.
The UK National Institute for Health and Care Excellence said in April, external there was "little or no evidence" painkillers made any difference to quality of life, pain or psychological distress.
"I wish I'd never been on them," Ms Jones said.
"I do not need the drug for pain. I need the drug because my brain and body is dependent on it."

Niki Jones says her pain has reduced hugely since she explored other treatments
Gareth Parsons, a pain expert and senior lecturer at the University of South Wales, said painkillers were "great for treating pain that is new or associated with a recent injury" but not if it remains.
Some people ended up on increasingly strong painkillers for long periods of time, creating a "pain circle of pain, lack of sleep, fatigue, rest, and more pain", he said.
The best way to tackle this was to reduce or stop taking painkillers, remain physically active and do activities that were socially and emotionally enjoyable, he explained.
Lost independence
Ms Jones had been a successful executive assistant for the British Horseracing Authority in London.
On Christmas Eve 2002 she began experiencing excruciating pain in the side of her face while sitting watching TV with her grandmother at the family home in Brecon.
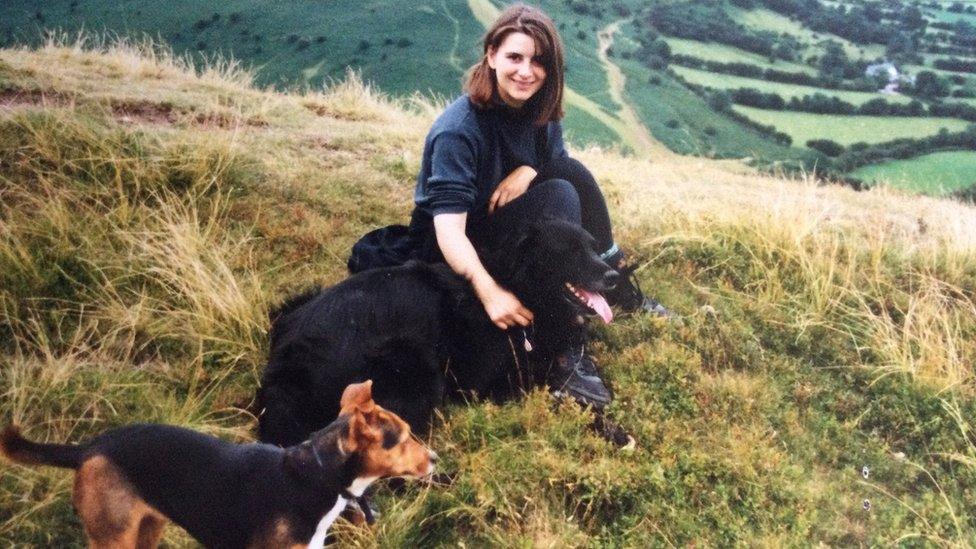
Niki Jones before she developed chronic pain
Doctors later diagnosed her with the sudden facial pain condition trigeminal neuralgia, external and Ms Jones began treatment with different drugs, operations and stronger medication.
The increasingly strong doses led the former keen horse-rider to quit her job in London and move back into her parents' house.
Once there her pain continued to worsen and as her medication progressively got stronger she was unable to work.
Her condition deteriorated so badly that at one point could only walk short distances with a stick, she said.
Doctors later prescribed her the high-strength synthetic opioid fentanyl, which she took through sickly sweet lollypops that "destroyed" her teeth, she said.
She said she was still "dependent" on the drug - which has claimed the lives of numerous people including pop star Prince - and became suicidal every time doctors tried to wean her off it.
Pain fell 'dramatically'
Despite her worsening condition, Ms Jones said it was only in 2019, after more than a decade of treatment, that a medical professional suggested she explore other avenues.
She took up ballet and began exercising, socialising and meditating as a form of treatment.
This led to her pain reducing "dramatically" in just three months, she said.

Niki Jones before she reduced her medication
Accepting her pain would not simply disappear - something she had hoped drugs would achieve - was key to her recovery, she said.
Ms Jones has since become an advocate for pain management and works with a group called Flippin' Pain to help sufferers manage the condition.
Despite her progress, she still has to take fentanyl patches daily, faces losing her teeth within the next decade and will have to have her gall bladder removed.
She said: "I've never misused drugs. I would stop tomorrow, if I could.
"If somebody said, 'you know you can stop tomorrow?' I would never touch fentanyl again.
"The government really should step up and support people because I'm far from the only person who has problems with dependency on drugs," she said.
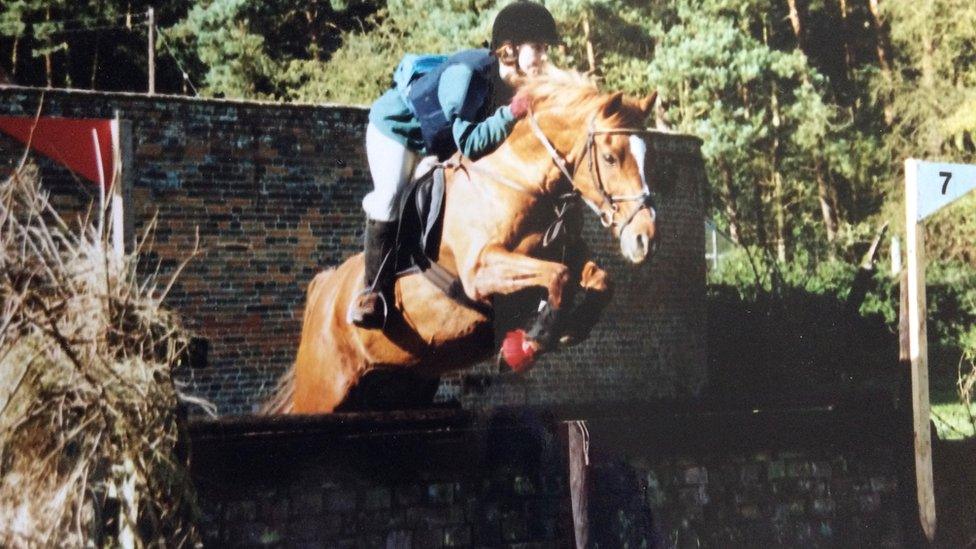
Niki Jones has had a lifelong love of horses
A Welsh government spokeswoman said: "A range of resources are available to healthcare professionals to help them help people make informed decisions about their care and support.
"This includes using non-pharmacological approaches wherever appropriate and avoiding the unnecessary use of medications.
"Where medicines are prescribed, healthcare professionals must make arrangements for regular reviews and for treatments to be stopped where they no longer provide benefit.
"We invest almost £55m every year to provide a range of services to respond to all forms of drug and alcohol addiction, including addiction to prescription and over-the-counter medicines," she said.

KEEPING FAITH: Binge-watch the the third and final series
LAND OF THE WILD: SECRETS: Explore the hidden world of Welsh wildlife like never before

- Published27 June 2021

- Published4 August 2020

- Published19 April 2021

- Published15 January 2021
