Covid: Pressure on ICU staff concerning, Hywel Dda consultant says
- Published
- comments
Covid: Intensive care consultant at Glangwili hospital describes pressure
The pressure on intensive care staff is as high as it has been since the pandemic began, a leading consultant has said.
Dr Michael Martin, of Hywel Dda University Health Board, said patients with other conditions on top of Covid patients is making the situation worse.
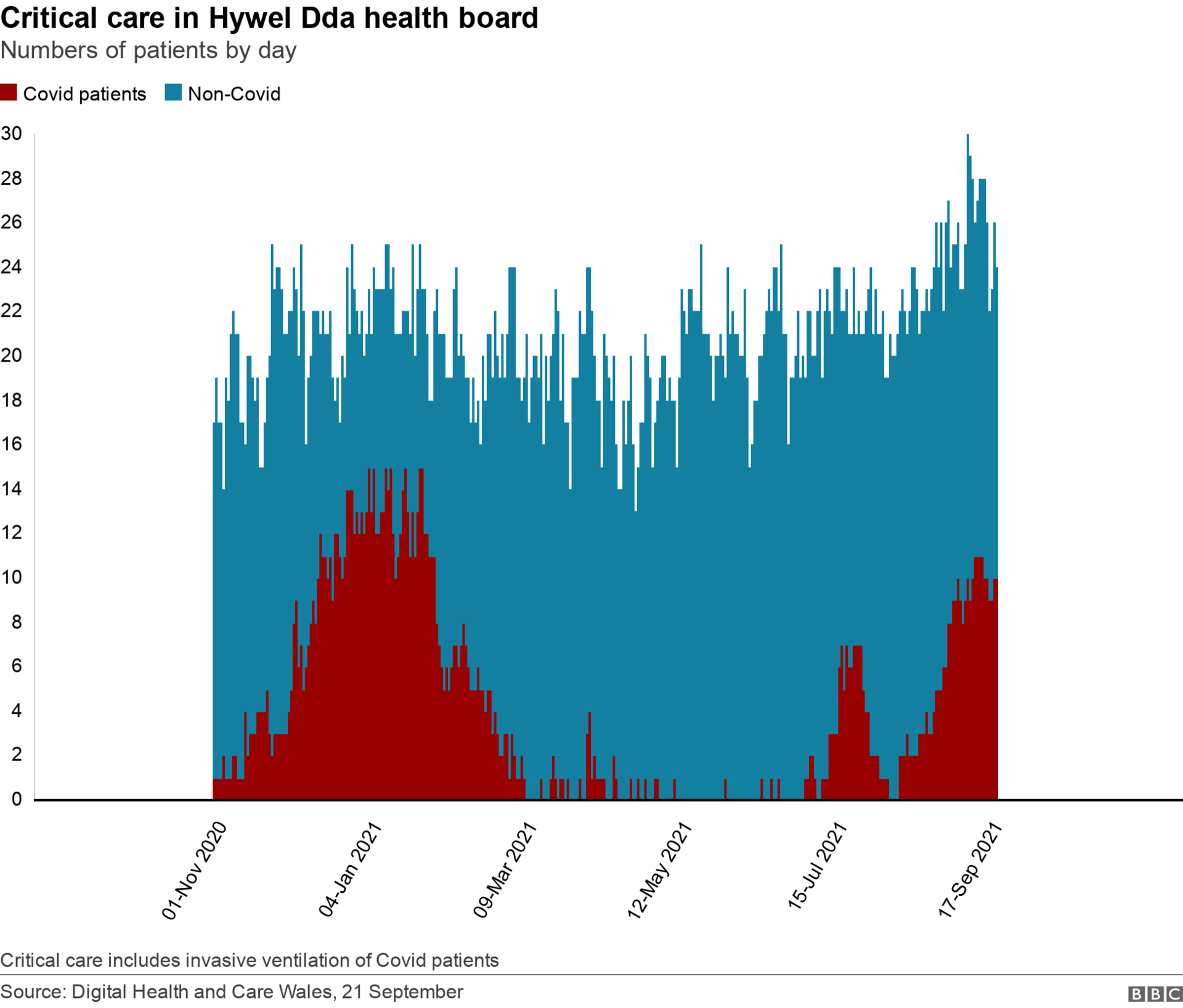
Ten of about 24 critical care beds in its hospitals were occupied by Covid patients on Monday.
Staff shortages have made him dread the winter months, the doctor said.
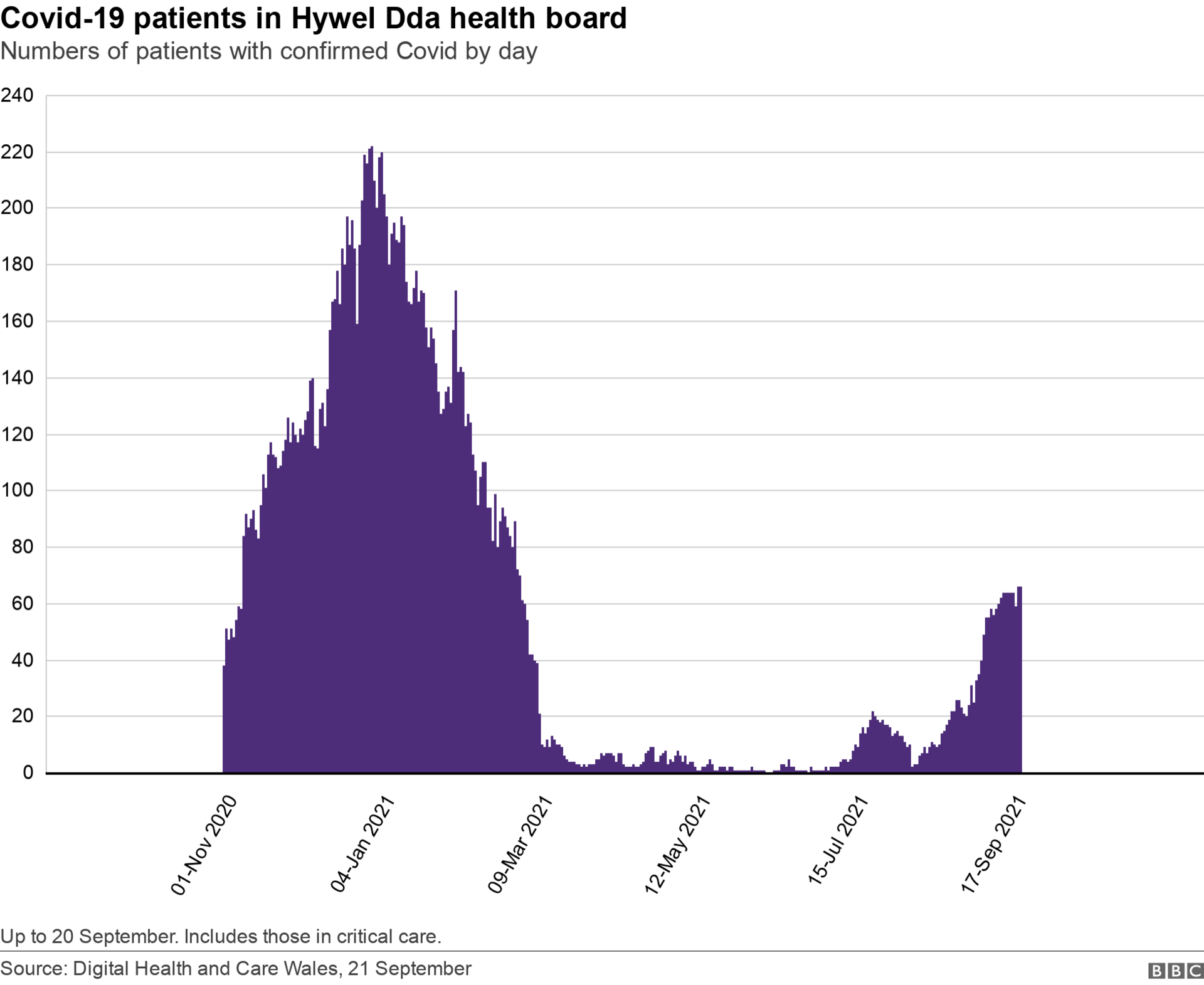
Covid cases in the Hywel Dda area, which covers Ceredigion, Pembrokeshire and Carmarthenshire, have been rising with planned surgery suspended in some hospitals due to Covid pressures.
Dr Martin said west Wales' infection rates compared to the rest of Wales were "much lower" in the first two waves.
"Now it's probably more than what we had throughout the period when it was difficult in the first two waves, especially for Glangwili hospital as we've tried to centralise things a bit more," he said, adding staff are "burnt out".
"Here, in Glangwili hospital, the emergency hospital for west Wales, it's a difficult scenario because we basically lose more than half of our intensive care beds.
He said Covid patients means "a lot of work for everybody - they're difficult", adding: "You don't just cure them in a couple of days".
The health board said about half of its 12 Covid-positive patients are vaccinated.
While those that have been jabbed are seeing better treatment success rates, Dr Martin said he remains concerned about the number of patients coming into hospital already seriously ill with other conditions.

Dr Martin has written to Hywel Dda heath board expressing concern for the current situation at his hospital
There are fears of a pent-up demand from people either reluctant to get help due to the pandemic or those who might have had difficulties being seen due to growing delays and waiting times.
He said cancer diagnoses are happening later, at end stage, when the patient is very unwell in intensive care.
"It never used to happen that way," he said.
He added that intensive care medicine is "good at reversing acute things" but "patients are getting worse and worse because nobody has looked into them because the heath service has been busy [dealing with the virus]".
Dr Martin thinks that despite a high take up of vaccinations, the pressure on his hospitals is likely to remain high throughout the winter.
He questioned how people will deal with Covid if it "restarts" in the winter "because of all the patients we're seeing that the health service has not been able to deal with".
"For me, personally, that is more emotionally difficult to deal with at the moment."

Exhausted nurses
Nicky Hughes, associate director of the Royal College of Nursing in Wales, said some of her members were at "breaking point".
"Our nurses are telling us they are exhausted, they haven't had the chance to get over any of the last 18 months, they haven't had a let-up, every time they think there is a let-up, they are asked to do more and more," she told BBC Radio Wales Breakfast.
"We talk about resilience but how can you be resilient for two years at this level? It's just not going to work.
"Health boards need to make a decision on what services are priority and they need to priorities the safety of their staff," she said.
Covid 'perfect storm'
Dr Olwen Williams, who is vice president for Wales at the Royal College of Physicians, said Covid had exposed the lack of adequate staffing before the pandemic hit, and a mounting backlog of treatment and care.
"Health boards are being asked not only to upgrade their ability to reduce the backlog, but also try and tackle the rising cases of Covid, and keeping the two streams of work separate," she said.
"We really need some compassionate leadership here to ensure there is value for the NHS workforce, that they are getting the rest they need to face what could be an incredibly difficult winter, especially if we have a flu pandemic."


On the front line, for Dr Martin one of the biggest challenges he faces is having to deal with staff shortages.
He said burnt-out senior staff are choosing to leave intensive care for a "better work-life balance", causing him constant difficulty trying to fill rotas.
"After two Covid waves, a lot of doctors and nurses are trying to get out of intensive care. They simply don't want to do it anymore, they're burnt out, it's been emotionally draining."
He said very junior nursing staff are on ITU because of shortages and trying to convince junior doctors who are overworked to come in for extra shifts is "more difficult than the clinical work".
"At the moment, that is one of the most difficult aspects of the work."

THE LONG WALK HOME: 20,000 miles, 4 years, 1 man
MOTHERS, MISSILES AND THE AMERICAN PRESIDENT: The story of Greenham told like never before

Related topics
- Published16 September 2021

- Published11 September 2021

- Published10 September 2021

- Published2 September 2021

- Published15 November 2021

- Published28 May 2024
- Published2 April
