Covid: NHS Wales planned care will slow down - health minister
- Published

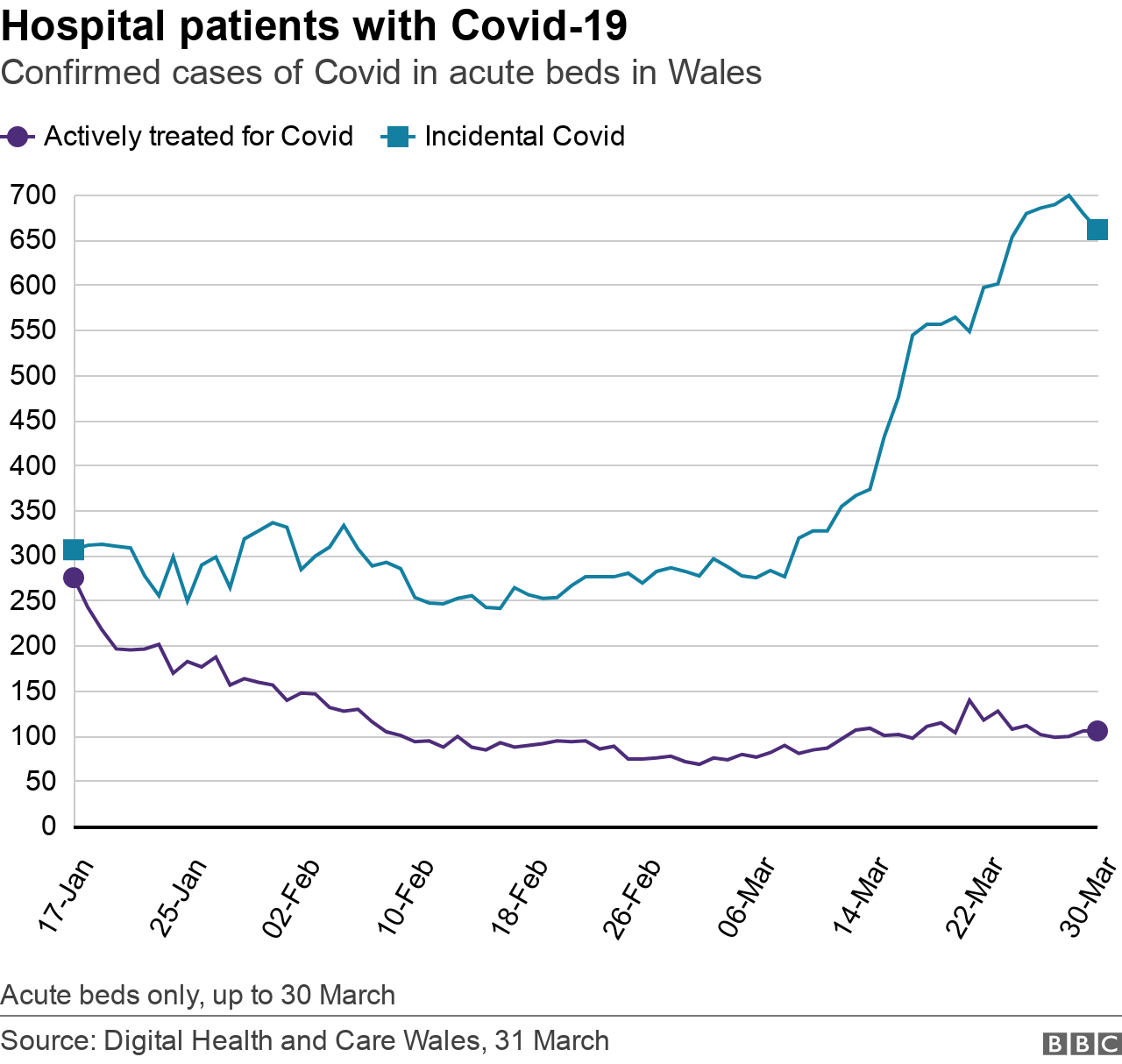
There was a rolling average of 939 hospital patients with confirmed Covid on 29 March
Planned treatment across the NHS in Wales is expected to slow down due to Covid, the Health Minister has warned.
This could cause a further rise in the record number of people waiting for non-urgent operations like hip replacements or cataract surgery.
Ms Morgan said pressure on the health service hadn't been seen on this scale since March last year.
"Something has to give and at the moment it probably is planned care," she said.
Rising Covid cases have led to limited bed capacity, staff sickness and difficulties discharging patients.
Ms Morgan said health boards have been forced to focus on what will "cause the least harm" by delaying planned treatments.
"I know that's a difficult message for people who are in pain and agony," she added.
What have Welsh health boards said?
In an attempt to relieve the pressure, all "non-essential activities" in the Aneurin Bevan health board area have been cancelled.
The health board issued a "black alert" on Tuesday, urging people to only visit the hospital if absolutely necessary.
On Wednesday, Hywel Dda health board also "briefly" issued a black warning.
Its director of operations Andrew Carruthers said the hospital was now operating at a red alert level, meaning people should only attend A&E with serious or life-threatening conditions.
Cardiff and Vale University Health Board said both University Hospital of Wales and University Hospital Llandough were operating at a level of "extreme pressure".
It said: "Our emergency unit at University Hospital of Wales is extremely busy and we would urge you to only attend the department where absolutely necessary."
"Covid rates are amongst the highest we've seen during the whole pandemic," Ms Morgan said.
"A lot of our care homes are closing because of outbreaks of Covid - and that just means that everything gets backed up, and so we have issues in accident and emergency."
Previously Ms Morgan has said there were 1,000 patients in Welsh hospitals who are medically fit to be discharged, but a shortage of social care support meant they could not leave the hospital.
"GP services are also under extreme pressure at the moment with absentee rates there at about 14% which are really high as well," she said.
The health minister urged people to first seek advice from NHS 111, and only those with "life-threatening illness or serious injury" to go to A&E.
Allow X content?
This article contains content provided by X. We ask for your permission before anything is loaded, as they may be using cookies and other technologies. You may want to read X’s cookie policy, external and privacy policy, external before accepting. To view this content choose ‘accept and continue’.

'Staff really struggling'
Darren Hughes, director of the Welsh NHS Confederation, echoed Ms Morgan's plea to use local services before attending A&E to help "exhausted" NHS staff.
"We're seeing that staff absences have gone up. We're at the limit in normal times but when you see a level of increase in absences because people being infected, it's having an enormous impact," he said.
"They've been working at the grindstone for two years and we need to give them a huge thanks."
Mr Hughes acknowledged how "tough" it is for people who are enduring long waits but urged them to do "everything they can to look after themselves".
He told BBC Radio Wales: "A&E is probably, in most places, not the best place to be. Seek advice from your community pharmacy, look at 111 services online, contact your GP and keep yourselves well as well."
The Welsh government said it had invested an extra £42m for social care and an additional £25m in urgent and emergency care, on top of £248m already announced for the NHS Covid recovery fund.
Analysis: Figures show the NHS under pressure
We don't have daily figures for people using emergency units but we can see pressures on beds in certain health boards.
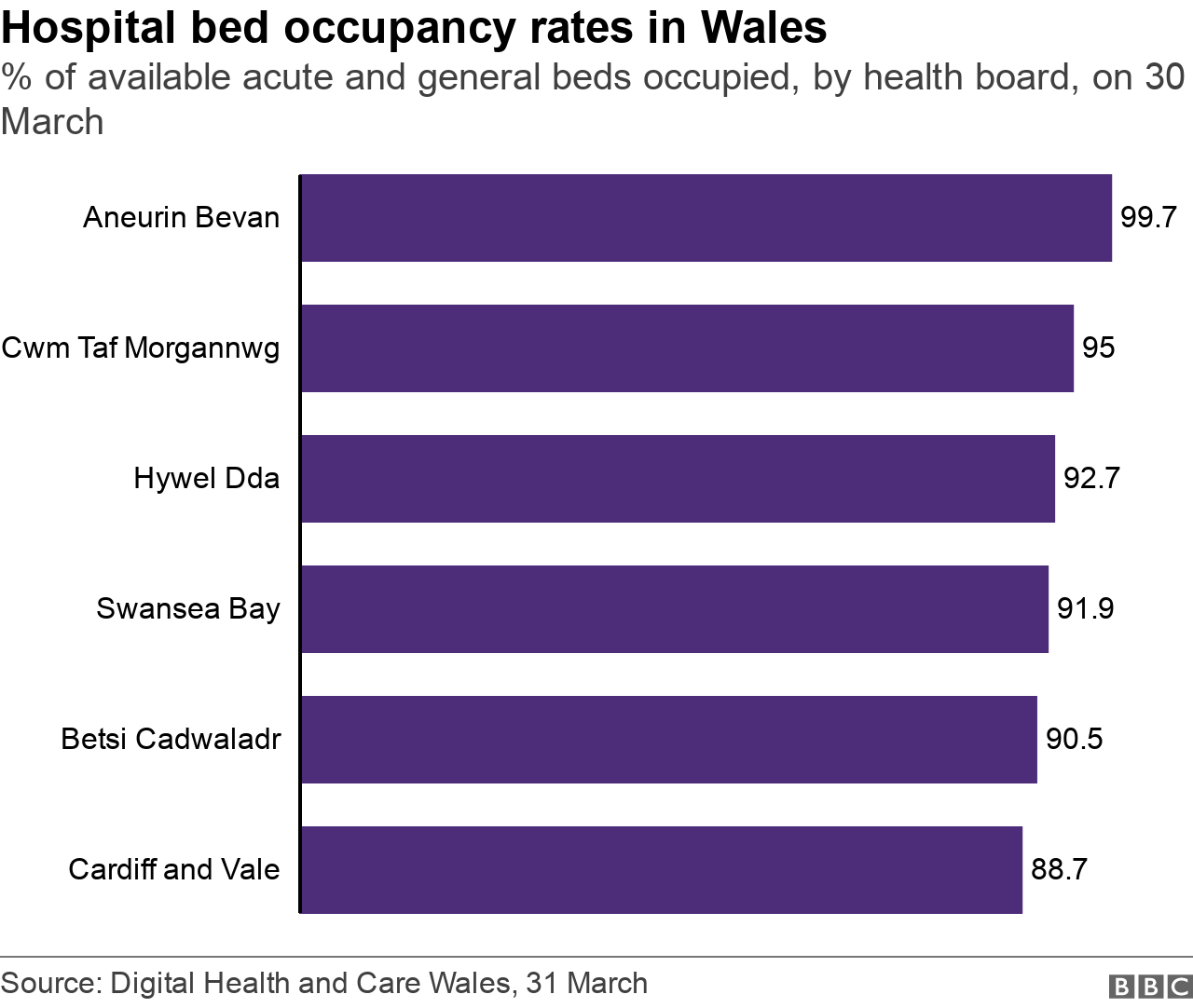
In Aneurin Bevan, there were only three available general and acute beds out of more than 1,000 in its hospitals since Sunday.
That's a bed occupancy rate of 99.7%, higher than the current Welsh average, which is just under 91%.
Although there were 144 patients with confirmed Covid in acute beds in Aneurin Bevan hospitals on Wednesday none were actually being treated for the virus, but for other conditions. It had one patient being treated for Covid who was in critical care.
The pattern in recent weeks is of most patients testing positive in Welsh hospitals for Covid being there to be treated primarily for something else.
This is a reflection of the Omicon sub-variant in the community, while there has also been a recent jump in infections caught while in hospital. Both can present a patient management challenge for hospitals, as well as potentially adding to complications for some patients.
Even in Cardiff and Vale, less than a quarter of its 187 acute patients with Covid were actively being treated for the virus. Its acute bed occupancy rate is lower, about 89% of beds are full.
Hywel Dda also has 98% of its patients with Covid being treated for other conditions. Its acute bed occupancy rate on Wednesday was 92%.
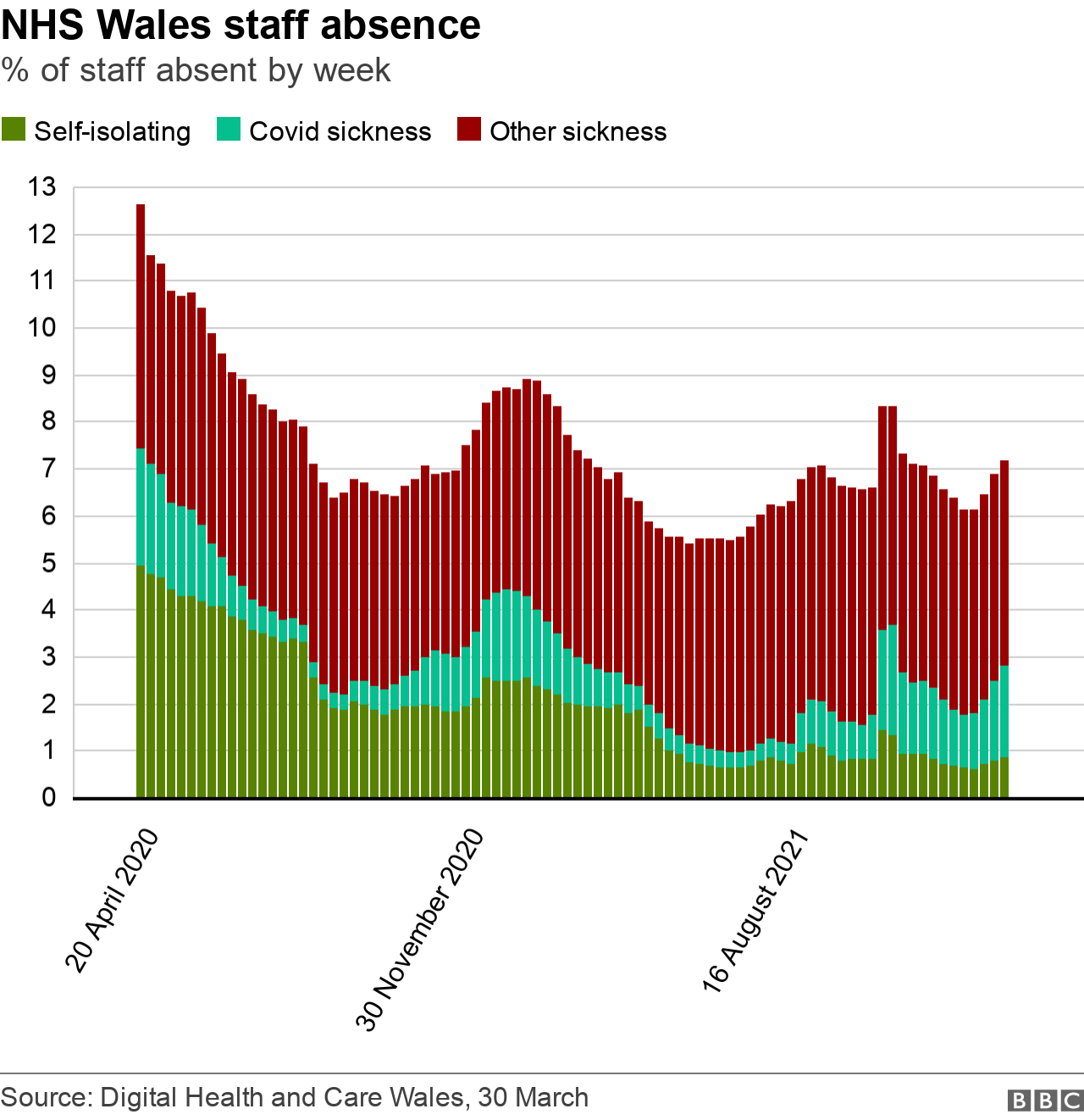
When we look at the latest NHS Wales staff absence figure - up to 28 March - this shows 7.2% of staff absent, the highest proportion since mid-January. Of these, 2.9% are linked to Covid or self-isolation.
This is still a lot less than during the two main peaks of the pandemic but will add to headaches for hospital managers.

HOW COVID MADE THE SENEDD MATTER: Welsh politics and politicians became interesting
LESSONS FROM LOCKDOWN: How has the experience of lockdown changed us?

- Published28 May 2024
- Published30 March 2022

- Published24 March 2022
