NHS Wales: Ambulance handover delays treble in two years
- Published

More than a quarter of a million hours in delays have clocked up outside A&E in the last year in Wales
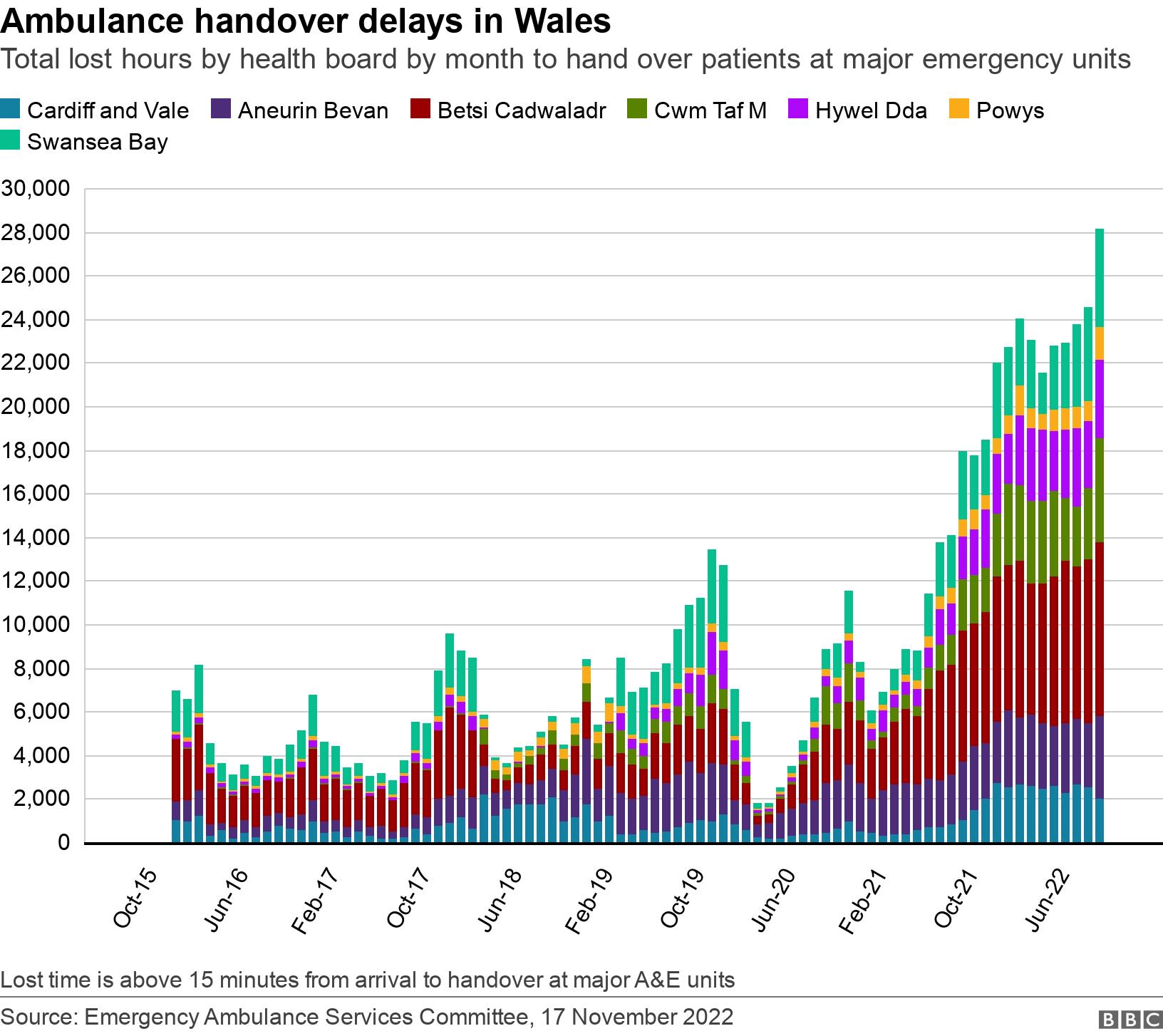
The number of hours ambulances are spending outside Welsh hospitals waiting to hand over patients has more than trebled in the past two years.
October saw a record 28,143 "hours lost" as crews stayed with patients who were unable to be passed over to the care of major emergency units in Wales.
The clock for delays starts 15 minutes after an ambulance arrives.
A health watchdog last year found prolonged delays a "regular occurrence", external but hours lost have shot up since.
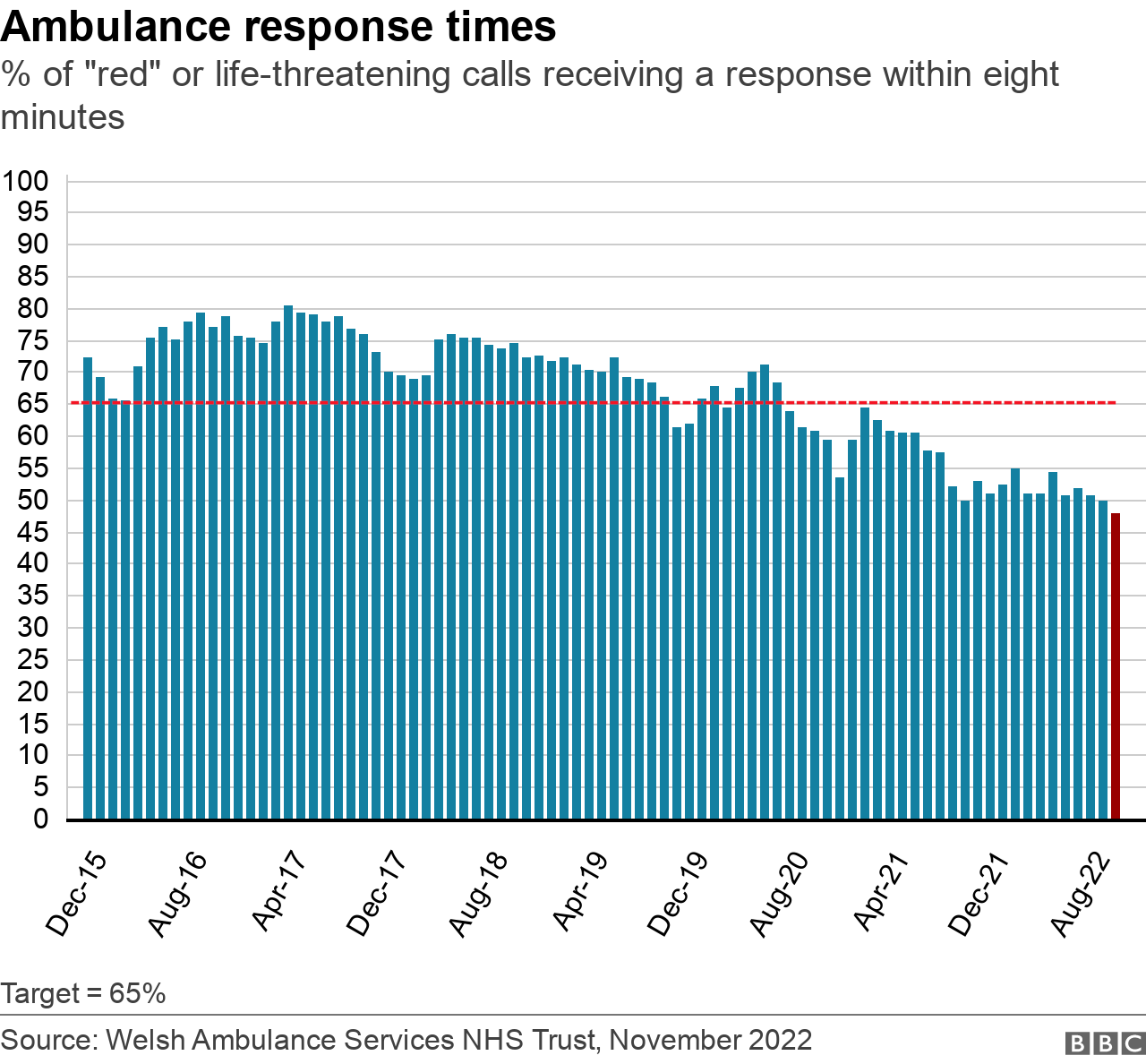
Meanwhile, ambulance response times are the worst on record.
They showed 48% of life-threatening red calls arrived at the scene within eight minutes, short of the 65% target.
Ambulance service managers say more than a third of vehicles in October had one patient in them outside a hospital, when ideally they should be out responding to other calls.
It's not unheard of for up to half of ambulances to be outside hospital at any one time.
A snapshot at one point on Thursday afternoon saw 42% of the 156 ambulances on the road outside a hospital waiting to hand over a patient.
What do the figures show?
The delays in handing patients over from ambulances through the doors of major A&E units have gone beyond 20,000 hours for all but one month in 2022
In October just 15.8% of patients taken to hospital were handed over within the target 15 minutes - the worst figures since these were first published in 2016 and the equivalent of one ambulance spending more than three years outside a hospital
"Lost hours" for patients were the worst on record in all health board areas, apart from Cardiff and Vale, with Betsi Cadwaladr in north Wales having more than 8,000 hours lost
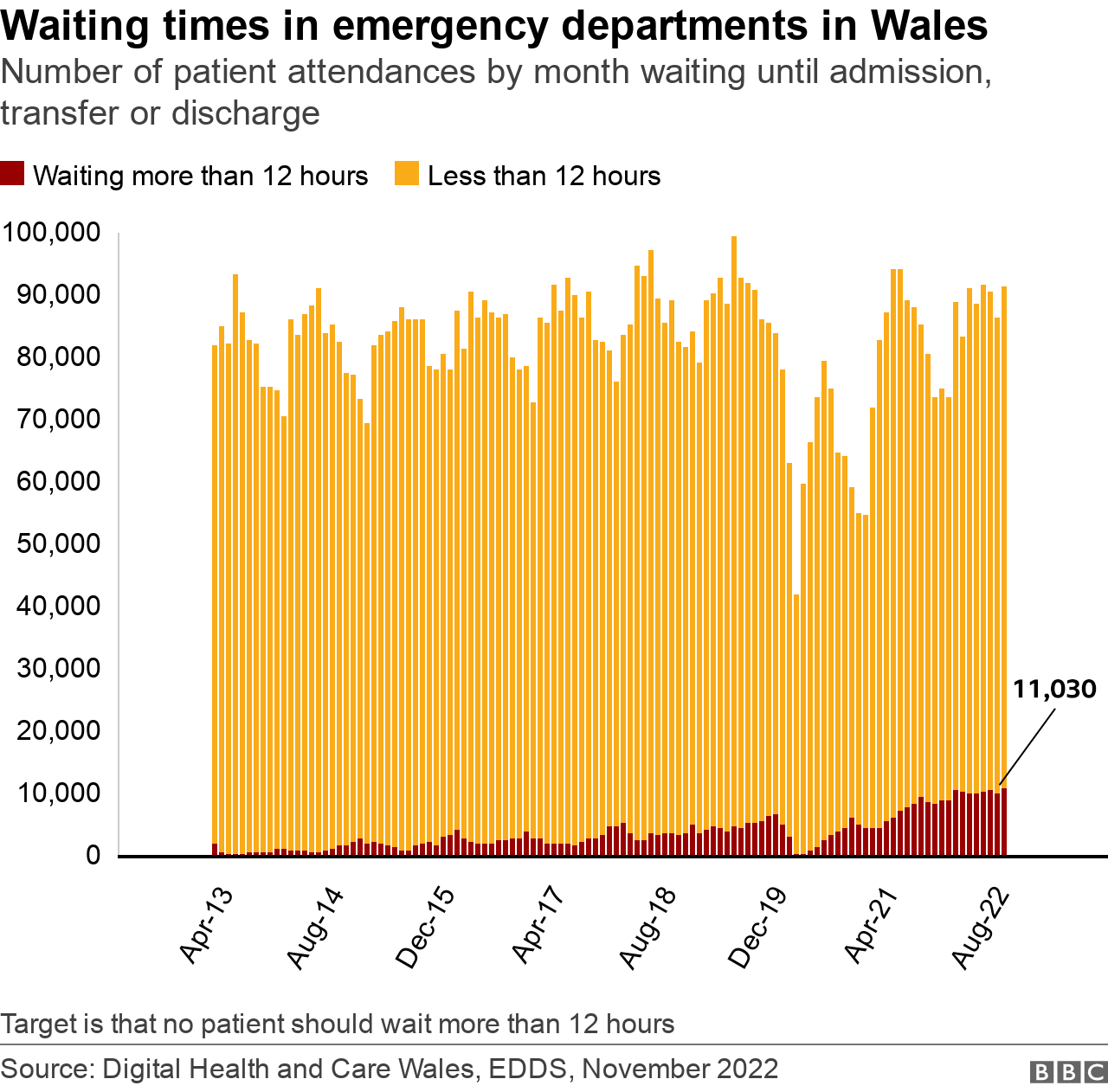
October saw the highest number of people waiting more than 12 hours in A&E - more than 11,000 - after nine of the 10 previous worst months on record
Since last December, there have been 11 months with the highest mean waiting times in A&E in a decade - peaking at an average wait of six hours and eight minutes - and at five hours 41 minutes in October.
Attendances at A&E hit 1m a year across Wales in the four years before Covid but they are still not quite at the numbers seen then
Higher proportions of patients in recent months have been arriving at A&E under their own steam, whether by car or taxi.
Chief Ambulance Service Commissioner for Wales Stephen Harrhy has the role of commissioning the right level of ambulance services.
"I've worked in the health service for over 40 years, and this is the most pressurised we've ever been," he said.
"The ambulance service is facing record levels of demand, as are other parts of the system.
"When the system is under such pressure, we don't run as efficiently as we should do."
"I can't justify the number of ambulance hours lost outside the hospital. I can't justify that."
He said more resources were being put in but there was not a "magic wand".
"I think everybody recognises the need to address flow, both in the hospital system at the back door and also pre-back door," Mr Harrhy added.
"So it's one of the key things that we have to deal with.
"And everybody's working as hard as they can to make sure that we do that."
Lee Brooks, director of operations at the Welsh Ambulance Service, said handover delays were the single biggest reason they could not get to some patients promptly.
"It's as frustrating for us as it is for patients when we can't deliver that part of our service."
He added that lost hours were the equivalent of more than a third of capacity for the entire month.
"Despite record recruitment, including the creation of 400 extra posts in our emergency medical service in the last three years, it is not enough to plug this lost capacity," said Mr Brooks.
The Welsh government acknowledged ambulance performance was "not where we expect it to be" but said it was driving improvements, including extending same-day emergency care services to open seven days a week, managing calls better to reduce hospital admissions, and recruiting more staff.
"Without all this the pressure on the system would be even greater," a spokesperson added.
Plaid Cymru health spokesman Rhun ap Iorwerth said the delays to ambulances were the "most explicit manifestation" of a clogged system.
"All areas are feeling immense strain," he said.
"While Covid has certainly exacerbated the problems, these issues existed long before the pandemic. Consequently, this isn't just about waiting to clear Covid backlogs - this requires long-term solutions to overcome long-standing problems."
Welsh Liberal Democrat leader Jane Dodds said: "What we need to see is real investment in primary health services in local communities, including our GPs to prevent these build-ups at emergency departments".
Welsh Conservatives said NHS Wales' ability to treat patients stood on a knife edge.
"I simply do not understand why Labour ministers are ignoring our calls for surgical hubs and winter war rooms to deal with these dangerously long waiting times when we see them leading to very visible progress in England," said health spokesman Russell George.


The sight of ambulances queueing outside hospitals has become commonplace.
For years there were seasonal fluctuations - peaking during the winter, dipping during the summer.
Yet this year even the lows are far greater than any peak we had previously seen.
The wider context is well documented and you need to look at the other end of the hospital journey to find its root cause.
Patients who are medically well enough to be discharged from hospital often have to remain on the ward because of a lack of social care in the community.
So those who arrive in A&E and are deemed to need a bed on a ward find themselves stuck in the emergency department as beds are not available further down the line.
It's this poor flow through the hospital system which means all those arriving in hospital A&E departments are likely to find long waits.

Kirsten Lapping said it was a frustrating experience in A&E
Last week, we spoke to Kirsten Lapping, from Cwmbran, Torfaen, whose partner was waiting 17 hours with head pains in A&E at The Grange hospital nearby.
There were about 150 people waiting at one point.
When all chairs and trolleys are already occupied, those arriving by ambulance may find the safest place for them to remain is on board, with the paramedics.
Recent initiatives have been introduced to release those crews should the most urgent, life-threatening "red calls" come through, but in many cases there was simply nowhere within the hospital for those patients to be placed.

What do the rest of the latest waiting times figures tell us?
Overall waiting times for hospital treatment have grown again to the worst on record - 754,677 patient pathways on the list.
The number of patients waiting more than a year for treatment is 181,482 - a 1% drop on last month's record figure.
Numbers waiting more than two years also fell - but there were 57,284 still waiting this long.
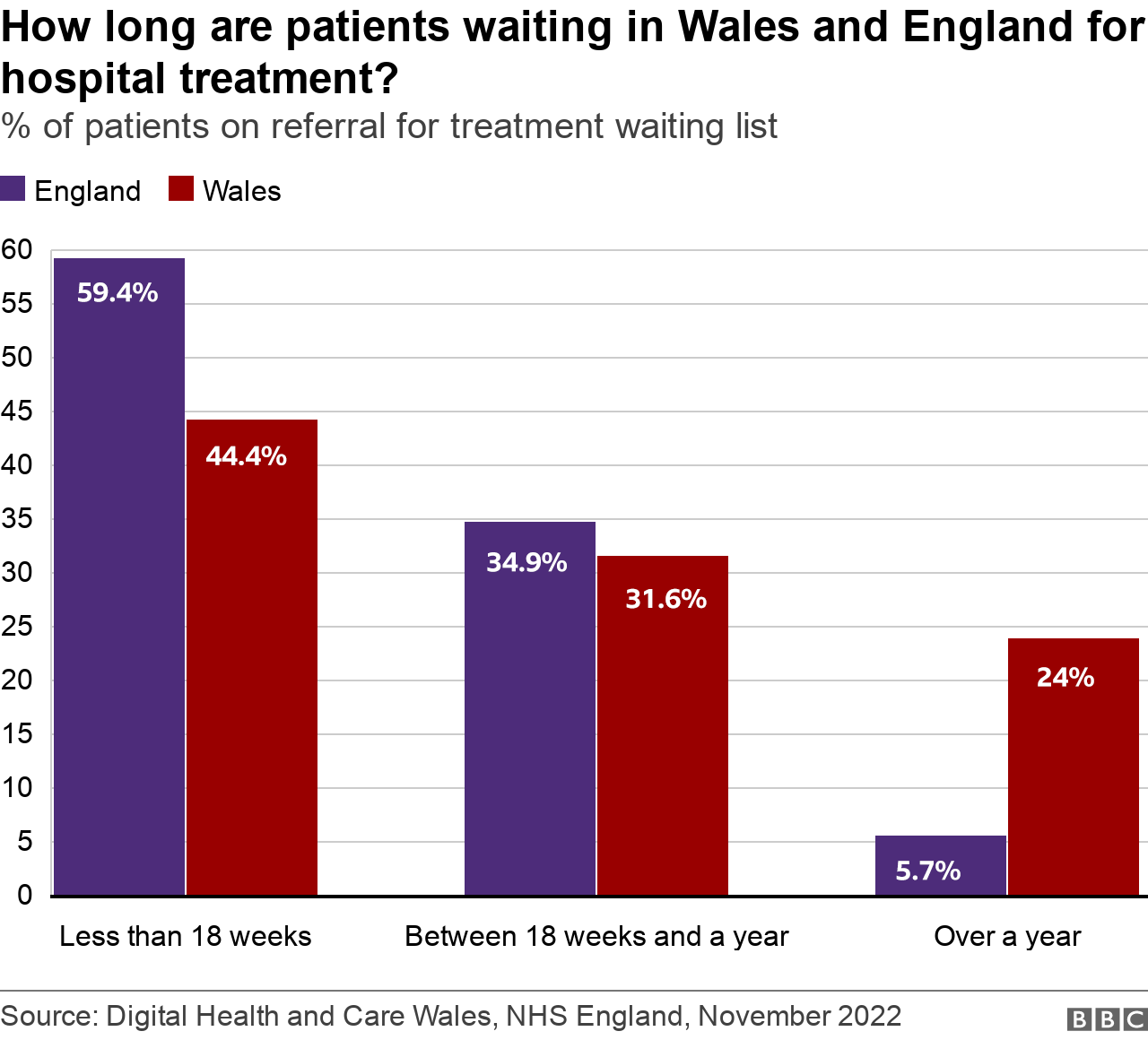
Looking at those longest waits for treatment, they show about a quarter of waits are more than a year in Wales - but that is less than 6% of waits in England.
About 7.6% of all waits in Wales are more than two years, while it's 0.03% of waits in England.
Two-thirds of patients were waiting less than the four-hour waiting target in A&E, a slight worsening in performance on the previous month.
But there were record numbers waiting more than 12 hours.
For cancer treatment, 53.3% of newly-diagnosed cancer patients started their treatment within the target of 62 days, an improvement on the 52.5% in the previous month.
'A miserable winter'
NHS organisations said the pressures on services have been made worse by wide-scale staffing shortages.
Thirty-six health and social care bodies have written to the first minister expressing concern over persistent problems with the recruitment and retention of staff which they said were crippling services.
The group, including royal colleges, charities, professional bodies and patients' groups said they faced a "miserable winter" and called on the Welsh government to publish a comprehensive workforce strategy outlining how it intends to fill gaps.
Dr Olwen Williams, vice president for Wales at the Royal College of Physicians said: "Staff shortages mean longer waiting lists. Yet despite repeated promises from the Welsh government, we still don't have a funded national workforce plan for health and social care - or indeed, any idea of when it will be published."
BMA Cymru Wales chair Dr Iona Collins said the waiting times figures were "simply not good enough," adding that "more money needs to be directed into frontline NHS services, so we can move away from record-breaking waiting lists for both emergency and scheduled NHS care".
The Welsh government said there were more staff working in NHS Wales than ever before, and it was investing record levels in training and professional education.
"The workforce strategy published by Health Education and Improvement Wales and Social Care Wales sets out our long term vision and actions for the health and social care workforce," said a spokesperson.
"We are also developing a shorter term plan to help deal with current pressures on our workforce."
- Published20 October 2022

- Published7 October 2021

- Published22 October 2022
