NHS Wales: Patient in hospital for weeks due to social care backlog
- Published

Roger does not know when he will be able to go home
"It would be much better if I was out there than in here," said Roger.
The 69-year-old looked wistfully across Newport from the window next to his bed at the Royal Gwent Hospital.
He has been here for three weeks after being admitted with an infection.
But although he is now well enough to leave and desperate to do so - he can't.
"I've still got a smile on my face, but I'm feeling a bit down," he said.
"I haven't got the foggiest when I'll be able to go home. I'm keeping my fingers crossed... because it will make a big difference."
Andrea and Adam Sheppard were on their way to Cwmbran's Grange Hospital when their child was born
Roger has cerebral palsy and the impact of his recent illness means he needs extra care to be arranged before he can safely go home.
Until then, he's stuck in a ward with no televisions. He watches whatever he can find on his phone.
Roger is not alone.
"At least a quarter of patients in our care of the elderly beds are in a similar position," explained Helen Price, a senior nurse at the hospital.
"It is very much a waiting game for that care to be available," she said.
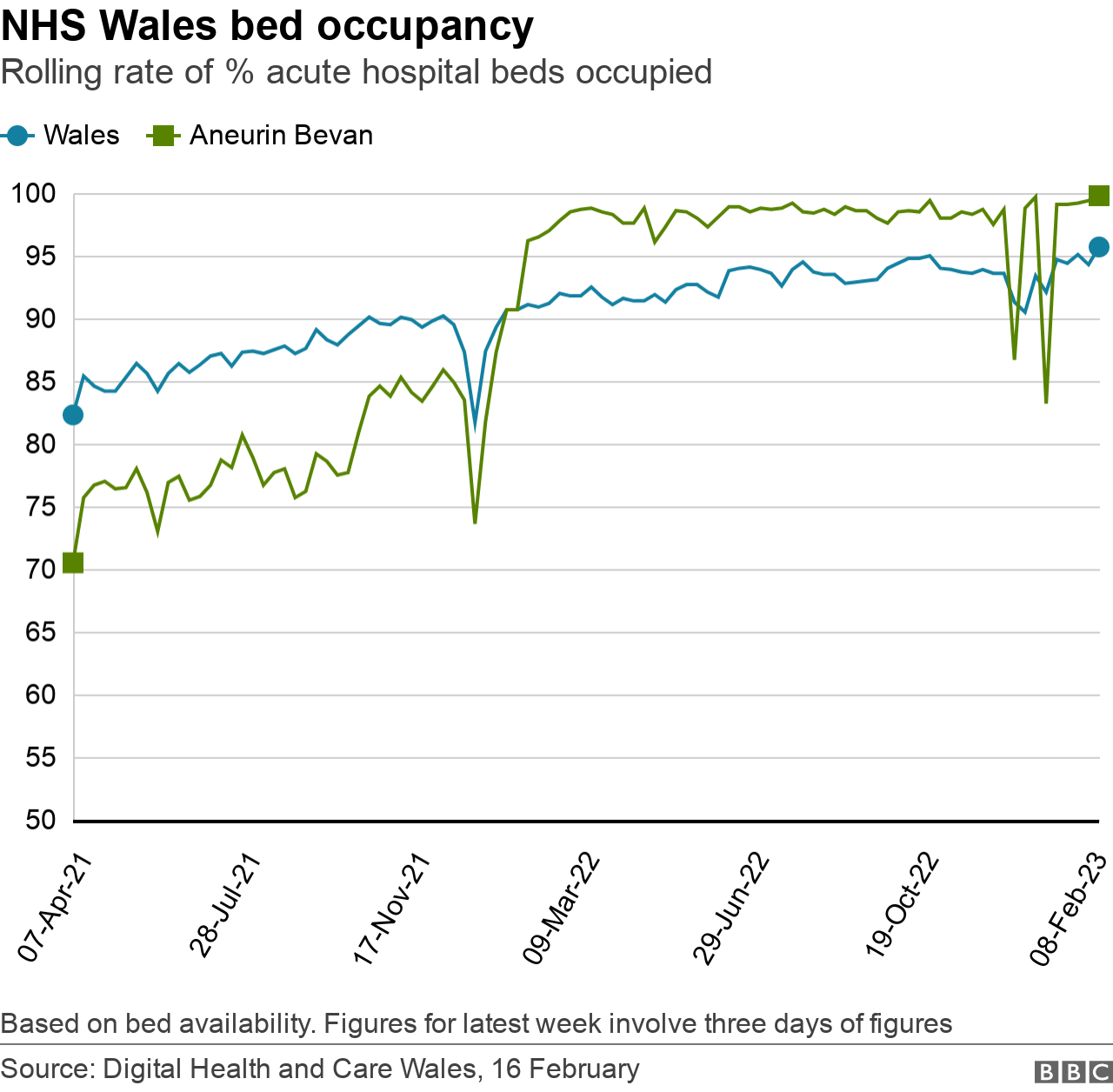
Hospitals in Wales are fuller than ever, according to the latest statistics.
This week, nearly 96% of all acute beds in the Welsh NHS were occupied, which is the highest figure ever recorded. In Aneurin Bevan, during most of the last week there have been only two available acute beds vacant - the occupancy rate hitting 99.8%.
These delays are having an impact not just on individual patients and staff but the work of the entire health board.
Paul Underwood, who manages urgent care in Aneurin Bevan University Health Board, said there are well over 350 patients medically fit enough to leave hospital.
"Roughly a third of patients do not need to be accommodated on those sites and that's extremely difficult," he said.

Paul Underwood says there are well over 350 patients well enough to be discharged
These logjams are often beyond the control of the NHS with social care largely the responsibility of local authorities.
But whatever the cause the impact on the health service is massive with hospitals fuller than ever.
For every patient like Roger waiting to leave, there are many more waiting for a bed to become available.
On the day of my visit there are only two acute beds free across the entire health board. Yet patients keep piling in.
At the Grange University Hospital in Cwmbran, six miles north of the Royal Gwent, I witness the impact in one of the busiest emergency departments in Wales.
At mid-morning the waiting room is already full, as are most of the department's beds or trolleys. There are 68 patients here in total.
'Some people abuse the system'
Frances Evans, 85, from Tredegar, is one of them. She is being assessed for a chest injury.But the day before, she had spent eight hours in the back of an ambulance outside the department.
"I was in the ambulance from 10 in the morning until six in the evening," she said. "And I had to come back and forth for the tests, it was really full."
Frances believes the NHS "has a lot too much to do" and that "some people abuse the system".
But I'm struck that staff say this morning is "relatively pleasant" compared to much of what they have experienced over the course of the winter.
'You feel like crying'
Lead nurse Claire Parkes said there have been days with more than 200 patients in the department, which she describes as "record-breaking numbers".
"The festive period was some of the worst I've seen in 25 years in emergency care," she said, adding that some patients were "waiting in chairs" for days.
"When you walk away you do feel like crying because you're not giving the quality of care that you want."
A Welsh government spokesperson said: "We are doing everything we can to help health boards improve flow through the healthcare system, including investing record amounts in health and care services.
"This winter we have secured more than 600 extra community beds and social care packages to help move people out of hospital to get care closer to home, and are working to deliver even more."
The importance of having spare capacity is made abundantly clear when a car screeches up to the A&E's front door.
In the passenger seat is a mother who has just given birth. Paramedics, nurses and doctors rush to help.
Within seconds, mother and baby are taken in Resus [Resuscitation], the part of A&E set aside for patients needing the most urgent care.
"That's a good example of why we always need capacity because we don't know what's around the corner," said Dr Owain Chandler, a consultant in the department.
"The danger would have been that there are times when we would have had to bring them into Resus without a cubicle ready, looking around to see who is the least unwell patient we can pull out... and doing that on the hoof."

The Grange University Hospital's emergency department is one of the busiest in Wales
But the outcome today is a happy one.
A few hours later I meet baby William on the maternity ward, along with his parents Andrea and Adam Sheppard as they are preparing to go home.
"There was no lack of anything from the staff," said Adam.
"The paramedic was there and soon there were four or five others at the door... plenty of staff to help."
Andrea agreed that there were "no problems", adding with a broad smile that "the baby is perfect".
The family will be forever grateful for the staff's willingness to go above and beyond despite relentless pressure.
A ray of light, perhaps, in what has arguably been the NHS's darkest winter.
WALES LIVE: Behind the headlines of Wales' biggest stories
WALESCAST: Your one-stop shop for Welsh politics

- Published3 January 2023

- Published8 January 2023

- Published28 September 2022
