Ambulance delays: Taxis sometimes the only option for patients
- Published

It is not uncommon for up to 30 ambulances to be stuck outside north Wales' main hospitals
Ambulance staff are being forced to book taxis to take patients to hospital when having suspected strokes or while experiencing chest pains.
And there are times when no ambulances at all are available across all of north Wales, according to a senior paramedic.
This is because so many crews are tied up outside full A&E departments.
The Welsh government said it expected health boards to make "urgent improvement" to reduce the delays.
The Welsh ambulance service insists it is trying hard to find solutions, including creating new paramedic roles dedicated to only the most serious calls.
But some staff feel they are swimming against the tide, with the most difficult weeks of winter still to come.
I spent two days with the ambulance service in north Wales and witnessed the relentless pressures first-hand.

Advance paramedic Aled Williams treats Jenny, who had a fall in the street
'Surely to God they can get an ambulance here quicker'
Arriving in Llandudno with paramedic Aled Williams, it is obvious that Jenny Evans, 80, is in considerable distress.
"I've been lying on the floor here for over an hour," she says, her head being cradled by a passer-by.
"Surely to God you can get an ambulance here quicker."
The ex-nurse and midwife is lying in the road after slipping outside her friend's home while delivering jigsaw puzzles for charity
A policeman is diverting traffic and it is feared Jenny has broken her thigh bone.
Neighbours and an ex-fireman with medical training help keep her warm on a bitterly cold afternoon.
Soon after we arrive Aled starts giving Jenny a combination of much needed pain medication.
"Unfortunately she does appear to have broken her hip," he tells me.
"We've managed to get on top of the pain now but obviously it's getting dark and cold so our priority is to keep her warm."
As a paramedic with specialist training, Aled can give more advanced treatments at the scene.
But working from a rapid response car means he won't be able take Jenny to hospital, and asks for an ambulance to come on blue lights.
The nearest available one is in Llangefni, 30 miles (48.3km) and 45 minutes away.
"Unfortunately it does happen. Patients wait longer than we would want them," Aled admits.
Jenny's ambulance finally arrives as night falls, and paramedic Andy Davies takes over from Aled.
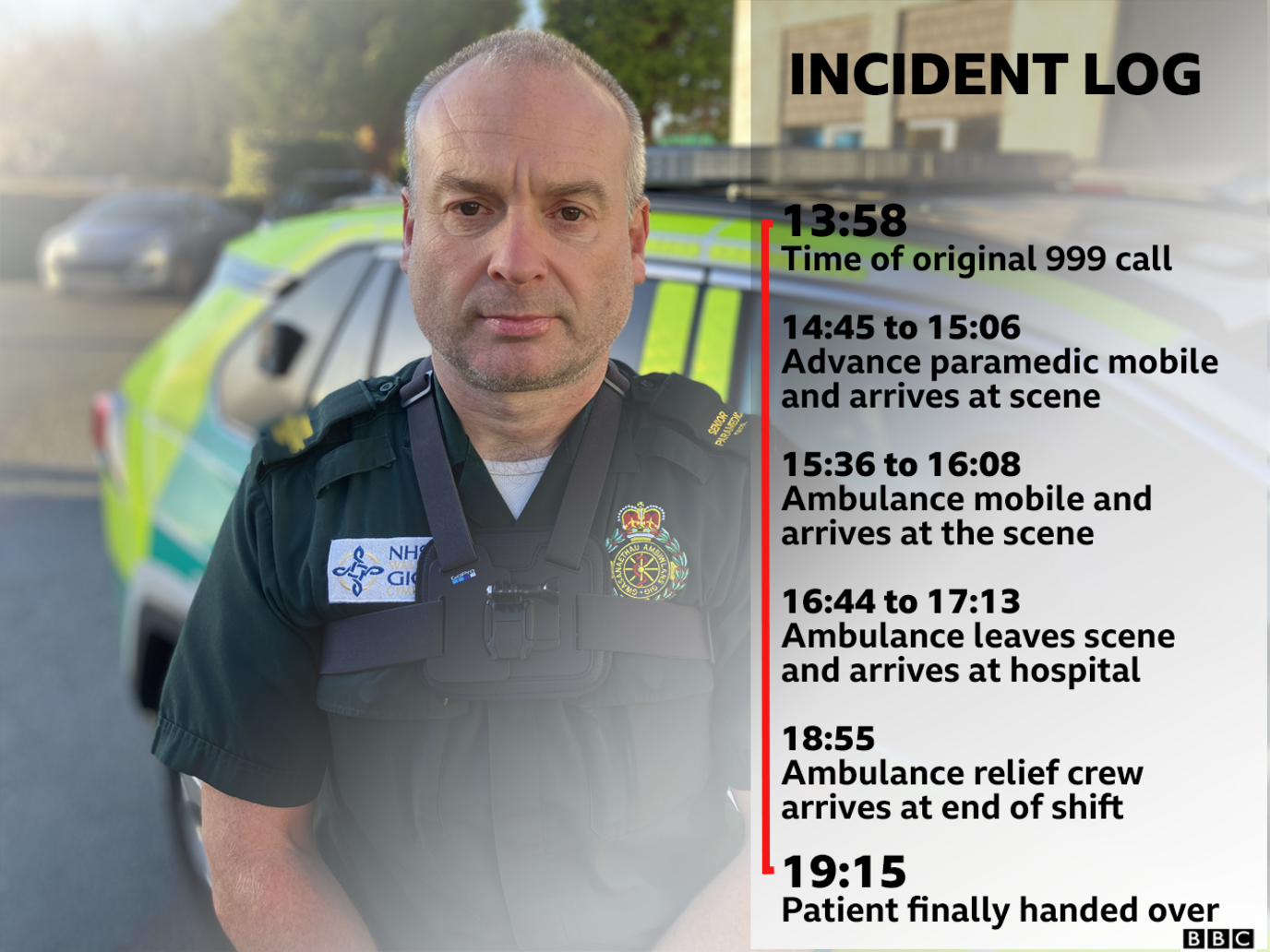
Aled Williams
They will soon be on their way to A&E, but it's likely Jenny will still have to wait hours before she can be handed over.
"It happens every shift," Andy tells me.
"I was outside Glan Clwyd hospital for 10 hours recently - it was my first patient and we stayed there for an entire shift."
He admits people can become verbally abusive "but there's nothing we can do to change it and it's heartbreaking to see".
Aled is one of around 100 paramedics in Wales who are trained as CHARU (Cymru High Acuity Response Unit) Paramedics., external
The idea is they are "ring-fenced" for the most serious calls.
The relatively new role was established, in part, because of concerns over ambulance delays on calls where lives are at immediate risk.
"It's not uncommon to have 25 maybe 30 ambulances stuck outside our three main hospitals in north Wales," he says.
That's a huge proportion considering at peak times the service has around 43 vehicles available across the region.

Dominic Egan says using a taxi or asking families is a last resort
'It scares me to work like this'
At the ambulance control room in St Asaph, staff give advice over the phone to less serious patients who might not need an ambulance.
But many of the calls are from genuinely very sick patients.
And because at times there are no ambulances free at all - staff say they have to ask families or even taxis to take very sick patients in.
"It may be [a patient with] chest pain where somebody might need an ECG or blood tests in hospital, right the way through to somebody with active symptoms of stroke," says paramedic Dominic Egan.
"When we don't have any resources available... just leaving [those patients] waiting longer and longer is only going to cause more issues for their health."
"So let's just get them there as soon as possible."
It makes me upset and doesn't sit right with me ... but sometimes we have no other option
But nurse Sian Stott says having to make those decisions can be distressing.
"It scares me to work like this, to make these decisions even though they might be the right ones [because of the huge pressures].
"I feel really uncomfortable asking for a taxi for someone who's having a stroke or asking their families to take them in by car.
"It makes me upset and doesn't sit right with me... but sometimes we have no other option."

Ann Williams waited outside a hospital in an ambulance for more than four hours
Outside Glan Clwyd hospital's A&E I get a sense of the scale of the delays first-hand.
Ann Williams, 78, is in one of eight ambulances queuing outside.
Belfast-born, the great-grandmother to no fewer than 130 children has lived in north Wales for 70 years, and worked for a time at Llandudno hospital.
Ann is putting on a brave face because she's in a lot of pain.
"We've taken her to the doctors quite a few times," her granddaughter Danielle Abbot tells me.
"But last night the pain got so intense we had to call the ambulance."
Almost four hours later the ambulance arrived at 07.52 in the morning.
It's now midday and Ann is still with the crew.
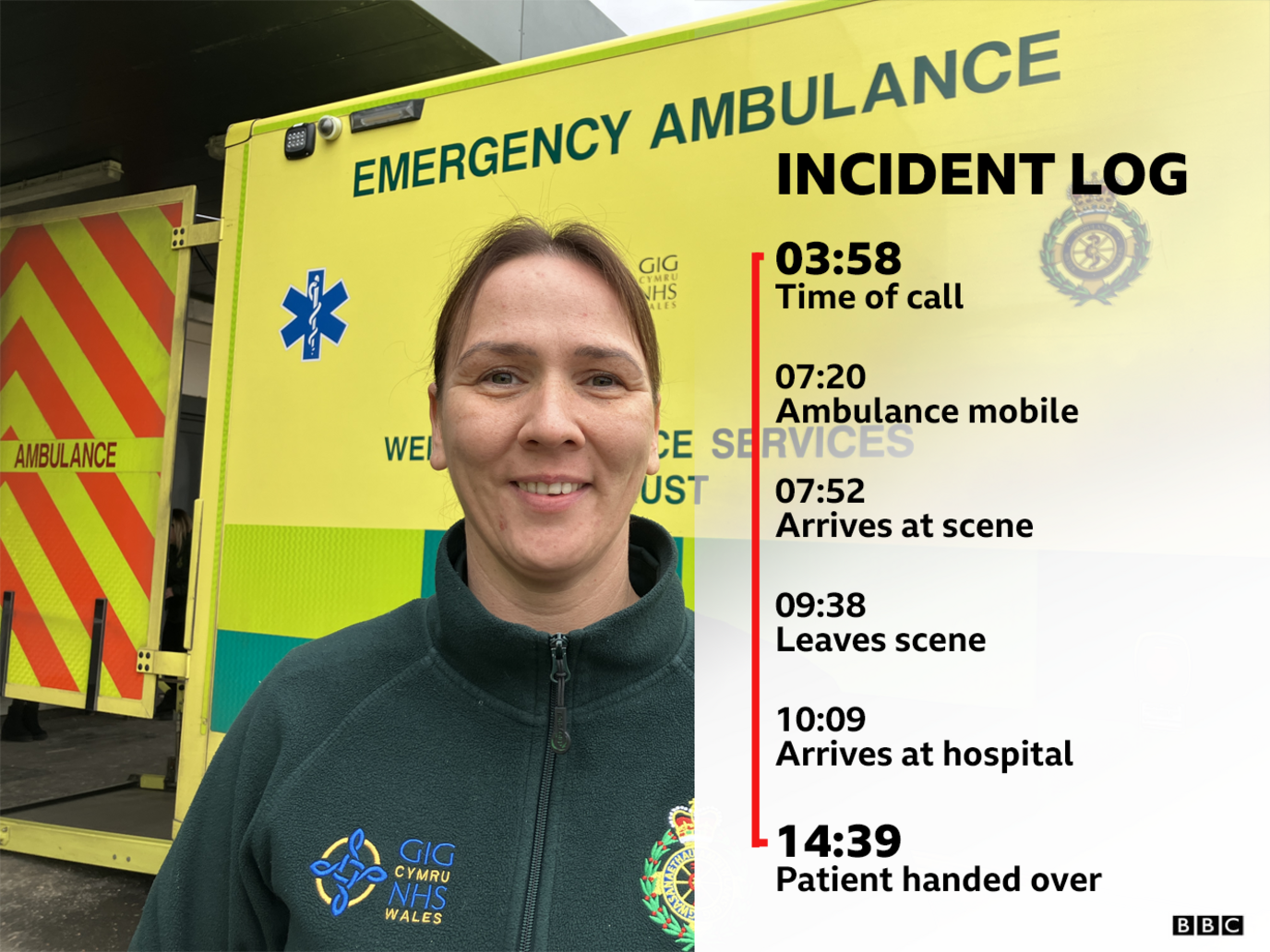
Calli Johnson
"It's quite normal now" says paramedic Calli Johnson.
"I should imagine we'll be here for the best part of the day. But some shifts we don't even go out to a job.
"We can come in straight to the hospital as the start of a shift to relieve a crew that's been stuck here all day and night."
She said it was disheartening "not doing what we're trained to do".
What do the figures look like?
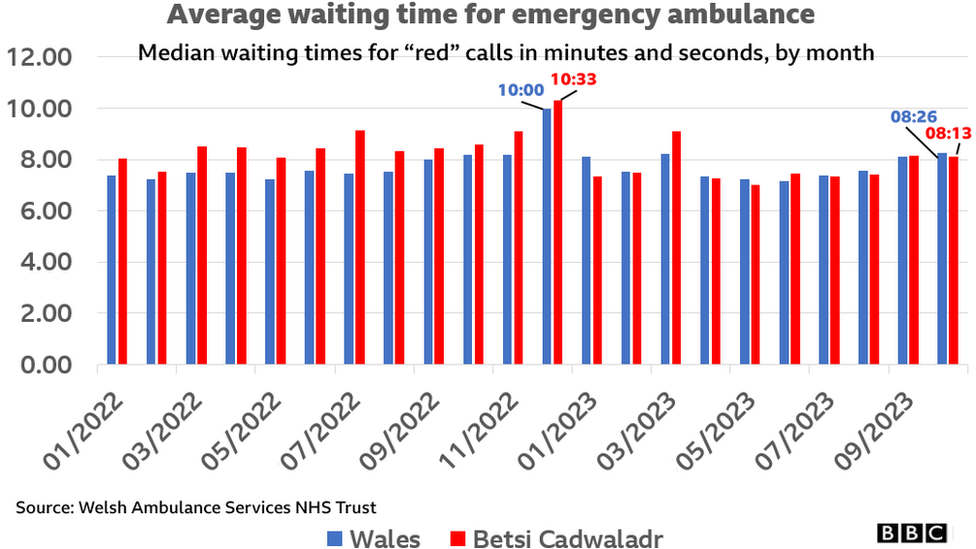
The average wait for a "red" call was eight minutes, 13 seconds in October. It peaked last winter when it was more than 10 minutes.
Red calls have been a growing proportion of those calls which need an ambulance response. In October, 19% of all calls were coded red and there were more than 1,000 in a month for only the second time. Five years ago, they made up 7% of calls (400 a month).
48.5% of "red" calls arrived within eight minute, slightly better than average for the fourth month running.
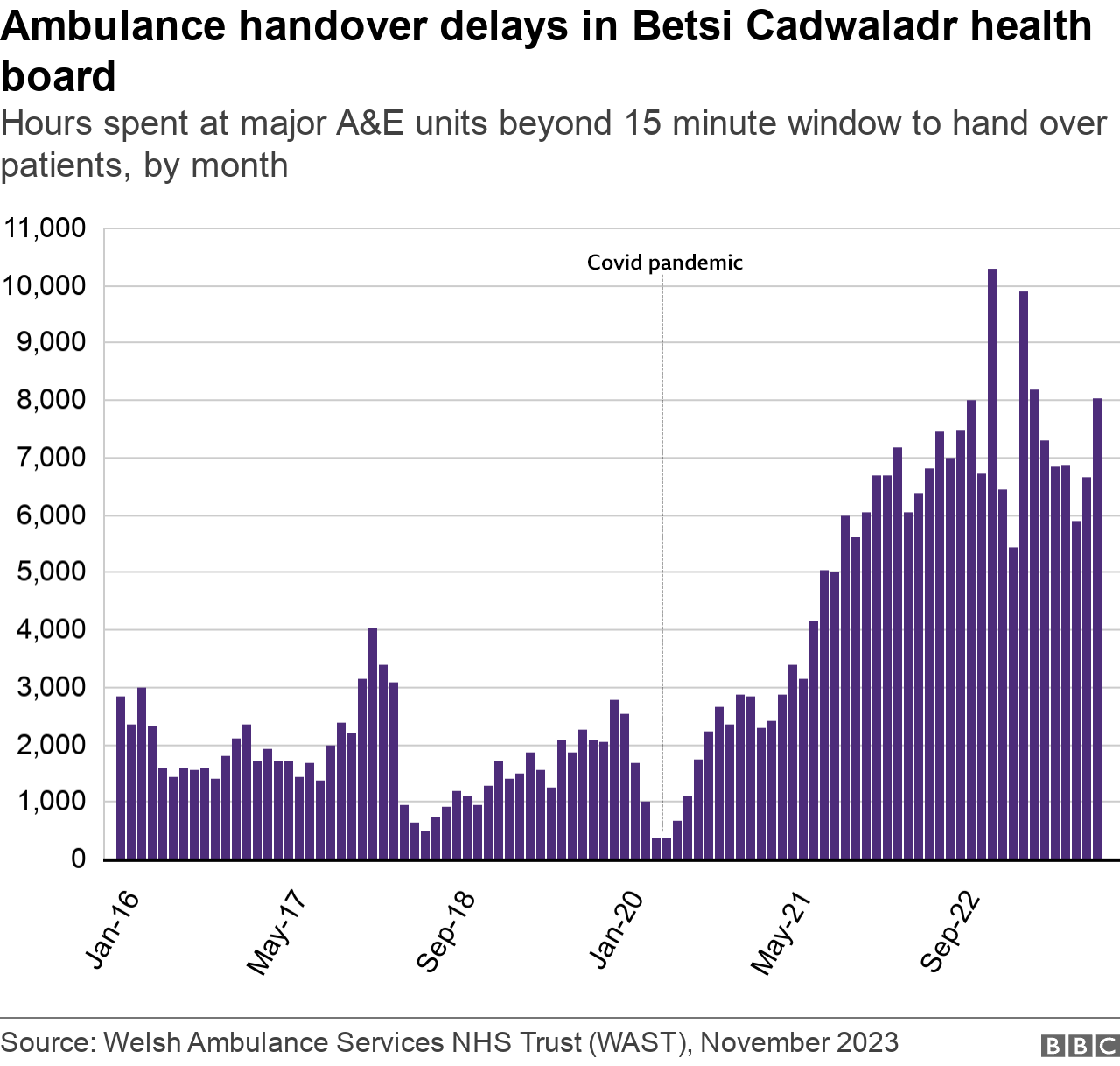
Handover delays have risen steadily since Covid. More than 8,000 hours were spent outside major A&Es in north Wales in October, above the 15-minute window for ambulances to hand over patients. Only around 17% of ambulances handed patients over within the window. This was worse than the Welsh average of 21%.
Betsi Cadwaldr health board says it's put a "number of measures" in place to alleviate long waits and says doctors liaise with paramedics to assess patients who have been waiting outside for long periods.
It says some of the reasons for the delays are beyond its control and are due to backlogs in discharging patients because of pressures on social care.
Out the Welsh NHS' 9,000 hospital beds, at any one time around 1,600 are taken by patients well enough to leave hospital.
But the Welsh government says it's been "very clear with health boards about our expectations for urgent improvements".

KEEPING IT UP: The big story of the little blue pill
IT'S MY SHOUT: Short films made by up-and-coming Welsh film-makers

- Published23 November 2023

- Published23 October 2023

- Published20 April 2023

- Published14 December 2023

