Minister orders spot checks into OAP Welsh NHS care
- Published

Lilian Williams' family described her treatment in hospital as "appalling"
Spot checks are to be carried out in hospitals in light of a report prompted by the death of an elderly patient.
The report, Trusted To Care, external, was ordered after the neglect of Lilian Williams, 82, treated at Bridgend and Neath Port Talbot hospitals.
Among several failings were patients being told to soil themselves and an ignorance of dementia needs.
Health Minister Mark Drakeford said he was "shocked, external" and apologised to those patients and families affected.
Mr Drakeford had originally ordered the report be carried out back in October.
It had followed criticism of Mrs Williams' care by her family and the public services ombudsman.
Hundreds of other families had made similar complaints over the treatment of their loved ones at hospitals run by Abertawe Bro Morgannwg University Health Board.
Published on Tuesday, Trusted To Care catalogued a series of failings at both hospitals.
It described "a sense of hopelessness" in the care of frail and elderly patients and cited "poor professional behaviour" as well as a "lack of suitably qualified, educated and motivated staff."
One patient told the review team: "I am in Hell."
Reacting to these findings, Mr Drakeford announced an immediate second review into the care of elderly people but this time looking at all major hospitals across Wales.
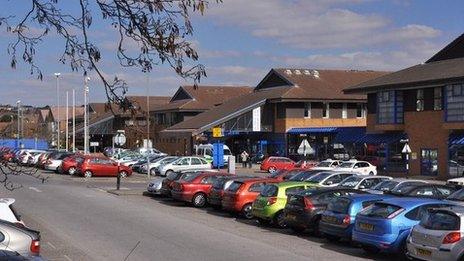
The Trusted To Care review was held after concerns at Neath Port Talbot Hospital and the Princess of Wales Hospital
A new task group will be led by the chief medical officer and chief nursing officer.
Referring to the report, Mr Drakeford said: "As the health minister, I give my unreserved apology to those individuals and their families whose care has fallen short of what they might expect from the Welsh NHS. I have been shocked by some of what I have read in this report.
"I am determined that nothing of this sort will be tolerated in these two hospitals, in this health board or indeed anywhere else in Wales in the future.
"I am not going to pick and choose parts of this report. The actions we need to make have been made clear and must be taken as a whole."
As well as elderly patients being instructed to go to the toilet in their beds, the report concluded that medicines had been recorded as given when they were not, and staff tolerated dangerous practice.
Among other findings were:
Variable or poor professional behaviour and practice in the care of frail older people
Deficiencies in elements of a culture of care based on proper respect and involvement of patients and relatives
Unacceptable limitations in essential 24/7 services leading to unnecessary delay to treatment and care
Lack of suitably qualified, educated and motivated staff particularly at night
Adversarial and slow complaints management
Disconnection between front-line staff and managers and confusion over leadership responsibilities and accountabilities
Problems with organisational strategies on quality and patient safety, capacity development and workforce planning
The report also says some staff felt ill equipped to meet the needs of patients with dementia
ABMU health board chairman Prof Andrew Davies is "ashamed" by care report
ABMU Health Board Chairman, Professor Andrew Davies, said, external: "As a health board we expect the highest professional standards and behaviours and will not tolerate poor care. This report was very uncomfortable to read but we are determined to emerge as a health board where all our hospitals provide excellent, patient-centred, care."
- Published13 May 2014

- Published13 May 2014

- Published26 July 2013

- Published25 July 2013

- Published29 July 2013