Bone marrow hope for African patients
- Published

Olabisi Bokinni (l) and Seun Adebiyi (r) had different personal reasons for their interest in bone marrow
Cancer dramatically changed the outlook of one Nigerian and prompted him to save countless other lives, writes US-based journalist Frederica Boswell, in this article published in the BBC Focus on Africa magazine
In August 2010, Olabisi Bokinni was 24 years old and working at a management consultancy in Ikeja, Lagos, when she learnt that her brother, who lived in the United States, was diagnosed with leukaemia.
"At the time, I did not have a clue about cancer," she says. After several weeks of tests and chemotherapy, she was told that his doctors were looking for a match for a stem cell donation to restore his weakened cells.
Doctors focused on his siblings, and sent a package for blood samples to be taken. Weeks later, Ms Bokinni was told that she was a possible match.
Her brother's hospital prepared her paperwork for a US visa, but it was denied. She remembers the day vividly: "The last thing I asked my interviewer was: 'You want him to die?'"
It was obvious that they needed another plan, so she was sent to the bone marrow registry in Cape Town, South Africa for the procedure.
When she finally saw the package of her stem cells that would be delivered to the hospital in the US, Ms Bokinni recalls pleading with the doctors: "Deliver it to save my brother's life!"
Family connections are the likeliest match for stem cell transplants. If a patient does not have a sibling, doctors search within the same ethnic group because there is a higher compatibility for certain genes called Human Leukocyte Antigen (HLA) markers.
This means that Ms Bokinni's brother could have found it difficult to find a donor in the US. African Americans make up only 8% of the bone marrow registry in the US, and according to the National Marrow Donor Programme, African-American patients have less than a 17% chance of finding a bone marrow match, compared to 70% of white patients.
Bone marrow registry
While working in the finance industry in the US, a Nigerian-American lawyer, Seun Adebiyi, was faced with these odds.
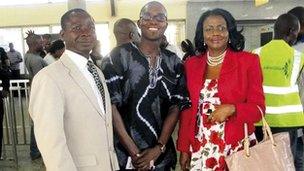
Mr Adebiyi (centre) joined forces with doctors Ocheni (left) and Okoye (right) to start the bone marrow registry
He was diagnosed with lymphoblastic lymphoma and stem cell leukaemia in January 2009.
"Chemotherapy would buy me time, but not save my life. I needed a system reset," he explains.
Unfortunately, this was not going to prove easy to find in the US, and so he started looking to the country of his birth.
Mr Adebiyi knew that one in five black people in the world is Nigerian, and the country is home to a quarter of Africa's population.
With almost 400 distinct ethnic groups, the size and diversity made it the perfect place to establish a bone marrow registry.
"I decided that I wanted to start a registry in Nigeria for diaspora Africans to be able to draw from a pool of donors," he says.
There was no registry or infrastructure in Nigeria to help with his goal, but Mr Adebiyi is not one to shy away from a challenge.
He passed the bar exam, required to qualify fully in the US, while undergoing chemotherapy. "I wouldn't take no for an answer," he says simply.
South Africa had the only other registry in Africa, and he made a deal with them to store his initial data.
While still searching for a match of his own, Mr Adebiyi made the trip to Nigeria with the goal of finding 10,000 donors.
He held the first drive at the Nigerian Law School in Lagos. After addressing about 400 students, he handed out information and testing kits, and wrote in his journal of the day: "I am crushed in a sea of outstretched hands. We are completely swamped. History."
Seeing the number of people who came forward ready to save lives convinced him that a registry would work.
He joined forces with two doctors at the University of Nigeria Teaching Hospital in Enugu - Ifeoma Okoye and Sunday Ocheni.
The greatest challenge in getting started was finding the funds to buy the necessary computers and software.
"Seun had to buy everything with his personal money," explains Dr Ocheni, while asserting that, "funds still remain our greatest challenge impeding the growth of the registry."
Dr Okoye adds to their list of challenges: Getting reliable internet access and trying to maintain an independent uninterrupted power supply.
"The main thing is, I am so passionate about it now, in a way that I was not passionate about my prestigious job on Wall Street," says Mr Adebiyi.
"For the first 26 years of my life, I had it all planned out. Then I felt that I was going to die for six months, now I am healthy again and ready to embrace life."
He has high praise for the doctors who are working with him, but hopes that one day he will be able to pay them a salary. "I don't need one because my own gratitude is enough," he adds.
Anonymous donor
Mr Adebiyi's drive and energy is fuelled by appreciation for his own donor. A Nigerian woman living in the US had a baby and found out that she could donate the umbilical cord blood to the public bank.
That simple act led to the eventual transplant that would save his life. Due to American regulations, he was unable to meet the woman or child who donated to him, but he says that he hopes "they hear my story and connect the dots".

The University of Nigeria Teaching Hospital in Enugu is home to Africa's second bone marrow registry
Mr Adebiyi is passionate about the benefits of cord blood for African patients and the growing success of these transplants has also made him think about how the opportunity to help patients with cord blood was literally being thrown away.
"I know so many mothers whose kids have died because they couldn't find a stem cell transplant. Just across the Atlantic Ocean, there were millions of cord blood units which are being thrown away as medical waste. It is heartbreaking and so easy to fix," he says.
His team in Nigeria decided to add setting up a cord blood bank to their efforts - something that he was told by an American medical doctor "would not happen in her lifetime".
Dr Okoye disagrees, asserting that she believes that a cord blood bank will be fully functional in the next year.
"There are already significant resources in place at the teaching hospital of the College of Medicine [the proposed site]. So we feel that only modest infrastructure enhancements are needed for a cord blood bank with a minimum of cost," she says.
Mr Adebiyi also believes that the information that the bone marrow registry and cord blood bank holds will allow Nigeria to connect with international donors and patients but he is still realistic about the road ahead.
"Nigeria did its first stem cell transplant last year. There are only six doctors who can do it in the country. The US has all the doctors and facilities but not the donors."
Millions of Africans suffer from blood disorders which could be successfully treated through transplants that will be available thanks to the fruits of Mr Adebiyi's team's efforts.
As the registry is public, patients from across the world will also be able to access potential donors. To date, the Bone Marrow Registry has received requests for donor searches for patients from Ghana, Kuwait, Singapore, Nigeria and India, and three potential donors were identified for the Nigerian patients. They are currently undergoing testing to determine their full compatibility.
Ms Bokinni met Mr Adebiyi nearly a year after her brother survived his transplant procedure. He was in recovery at the time.
"He hugged me and said: 'You are the closest person I can relate to as a donor since I cannot know mine. It feels like you donated to me'."
Dr Ocheni emphasises that stem cell donation "is very safe". Volunteers can choose to donate directly from their bone marrow, or from peripheral blood which is similar to giving blood.
New mothers can also agree to donate their child's cord blood immediately after delivery rather than just throwing it away.
"This will lead to double satisfaction for parents - bring a baby into the world, and keep a patient alive," he suggests.
Ms Bokinni, whose brother sadly lost his fight with leukaemia and died this month, says her fight to save his life was a "deep and fulfilling act".
"I don't know what your goal in life is, neither do I know your aspirations, but I want to let you know that I have never felt so much joy in the simple sacrifice of being able to give someone a second chance at life."
A version of this article appeared in the final edition of the BBC Focus on Africa magazine.
- Published14 March 2012
- Published9 May 2012
- Published15 February 2012