A South Sudanese psychiatrist's Herculean task
- Published

Dr Atong Ayuel is one of two trained psychiatrists in South Sudan
South Sudan is desperately in need of mental health facilities to treat people brutalised by decades of conflict, writes the BBC's Tom Burridge after visiting the world's newest state.
In South Sudan, a country of some 11 million people, there are only two trained psychiatrists.
Dr Atong Ayuel is one of those two, and the new head of mental health care in South Sudan.
The country's third trained psychiatrist apparently lives in London.
A stocky, determined mother of three, Dr Atong is ambitious about what she, and her team of just 20 trained mental healthcare professionals, can achieve.
'Imprisoned'
However on our visit to Juba's main public hospital, there were only 10 patients undergoing treatment, despite the fact that the people of this land have suffered so much.
The short history of South Sudan, which three years ago became the world's youngest nation, is scarred by violence.
"The scale of the problem is huge," says Dr Atong.
South Sudan is desperately in need of mental health facilities

Many mentally ill people are seen as security risks
During the current civil war, which broke out in December, thousands have died and hundreds of thousands have fled their homes. They now live in camps, often in squalid conditions.
It is in that context that Dr Atong says the number of patients is increasing and she simply does not "have the resources or manpower" to treat them all.
What is more, there was conflict in this land for decades before South Sudan's independence in 2011 and it has taken its toll on the people here.
Drive through the capital Juba, and you can spot men walking naked through the streets.

Life for displaced people is hard and those in camps face the threat of cholera and other diseases
South Sudan is one of the poorest states in Africa
"Some men are becoming violent, they start shooting each other," says Dr Atong.
"Some of them are having a full-blown post-traumatic stress disorder."
What is shocking to many outside of South Sudan is that mentally ill people are kept not in a hospital, but at Juba's main prison.
Human rights organisations have criticised the government and have campaigned for their release or transfer to another facility.
While we were in Juba, Dr Atong started working at the prison in order to assess those patients being kept there.
She told us some of them have already been released.
Officials at Juba prison did not allow the BBC team inside. But they told us that there were still 150 people with mental health problems, being kept at the prison.
'Spotting patients'
Dr Atong rejects the criticism from human rights organisations and foreign journalists.

Police go around Juba looking for mentally ill people
She argues that the patients are not kept in the prison as criminals, but for their own safety, and that of others.
"Mentally ill patients are people who are not predictable," she says.
However, the fact that the authorities in Juba say they have to keep patients in the prison because there is nowhere else safe enough to house them underlines how basic South Sudan's mental health system is.
The sight of dozens of policemen in military-style uniforms, with riot shields and long police batons, heading out to pick up the men with serious psychological problems who wander Juba's streets also seems primitive, when compared to the sensitivity shown towards the issue of mental health in more developed nations.
We accompanied the squads on their patrol through the streets of Juba.
But the role of the police is seen as an important part of the South Sudanese government's strategy of tackling mental health.
Only they can safely remove men, whose behaviour can be unpredictable from the capital's dusty streets, and take them to the hospital, where they can be treated.
At one point I ask Dr Atong, who is out on this patrol, whether the police have spotted a possible patient.
She replies that the police saw a scruffy man wearing overalls, but it turned out "he was a mechanic".
Gargantuan task
And when I questioned a senior police officer on the patrol about how he and his colleagues were able to tell if someone was mentally ill, or not, he said, with some confidence, that it was "because of the way someone was dressed, and the way they moved".
But aside from such sensitivities, when addressing the issue of mental health, Dr Atong and her small team of mental health care professionals are trying to tackle a gargantuan task.

Children receive lessons on how to cope with stress during lessons in camps

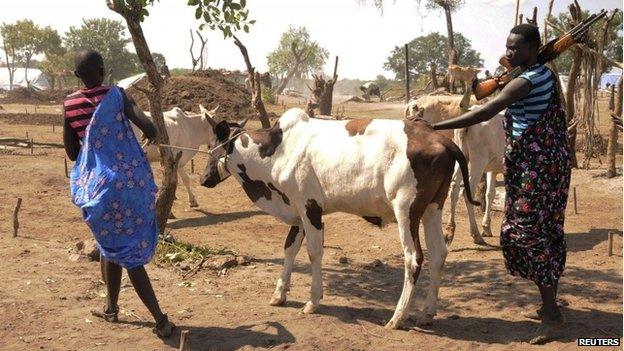
Both government and rebel forces are heavily armed
In a dilapidated corridor of Juba Hospital's mental health ward, I meet George who is visiting his wife.
He explains that a few days ago, his wife turned violent and was threatening to burn their house down.
But in some way they are the lucky ones. Reports suggest that other people in South Sudan, whose relatives suffer severe mental health problems resort to tying them up at home, because they have nowhere to take them for treatment.
Aid agencies also warn that treating mental health is crucial for South Sudan's future.
Heke Huisman, from the medical charity Doctors Without Borders, argues that if people who experience violence are not helped, then they themselves are more prone to turn to violence.
"If someone has been abused in his life, he becomes the abuser," she says.
And stories of trauma and tragedy are alarmingly common in South Sudan.
At a camp on the edge of Juba, where 1,700 people live who fled the recent fighting, we meet 12-year-old Mary.
In a sweet, innocent, high-pitched voice she recalls how both her parents and her two brothers were killed in the violence earlier this year.
Many believe that if South Sudan is to break-away from a self-destructive cycle of war, it must address the psychological cost of so much violence.