100 Women 2016: Fighting for a good death
- Published

Malawi is one of the world's least developed countries with very primitive health care. In March 1998, nurse Lucy Finch had visited her native Malawi to care for her sister who was dying of Aids, when hearing a young man's agonising death made her decide to come back and set up Malawi's first and only hospice.
In my view, the key ingredients for a "good death" are probably the same all over the world, in all cultures. The first is to know that you are about to die, not to have it hidden from you, and the second is to be kept, as far as possible, pain-free but alert.
This will give you the chance to prepare yourself, and those you care about, and thus approach your death with some equanimity. It is also preferable to be at home, and with close loved ones. This is your death, no-one else's, and you want to handle it your own way.
In sub-Saharan Africa, although all of the above would be desired, the access to a pain-free death is highly unlikely unless you are near to a centre like ours at Ndi Moyo.

Local hospitals are extremely under-resourced
My own commitment to bringing the possibility of a pain-free death to my native Malawi began one night when I was spending time with my sister who was in hospital.
In the next room, a young soldier was dying in terrible agony because no-one had the drugs necessary to relieve his excruciating pain. I will never forget listening to his harrowing screams, as, all alone, he faced both suffering of such intensity it was tearing his very being apart, and the terror of the unknown journey into death ahead of him.
That poor young man, though he never knew it, changed my life and indeed the lives of the many others who were to be helped by the palliative care I determined that night to introduce.
How hearing a man die in agony gave me a mission
The scourge of the HIV/Aids pandemic which swept sub-Saharan Africa in the 1980s like a biblical pestilence made more urgent than ever the need to assist people to a pain-free death.
The aggressive cancers associated with HIV did not carry off the elderly, but the sexually active age groups - the young and middle-aged. Unless palliative care could be introduced, the chances of a "good death", pain-free but alert, were minimal. And that is how we started.
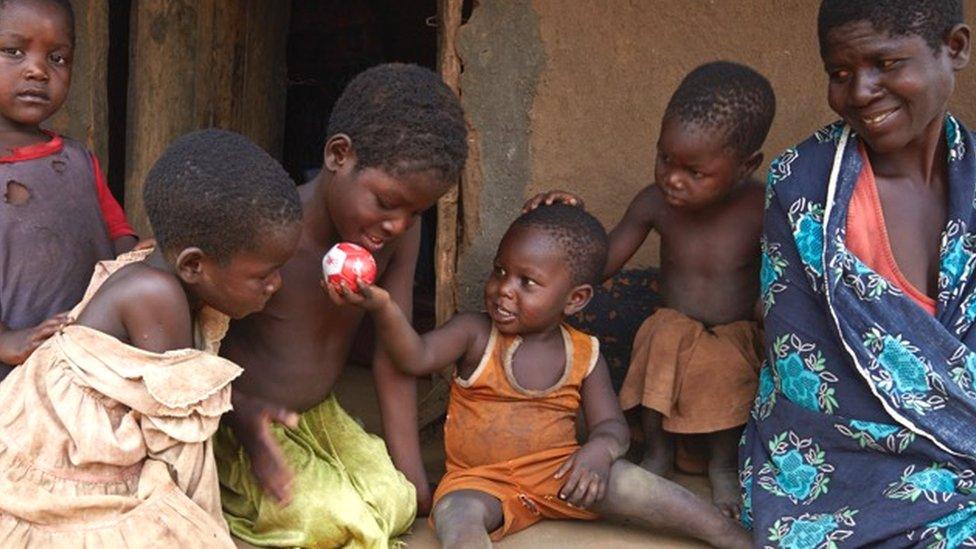
Unlike hospices in the West, we operate what we call "hospice at home", and at our out-patients facility. Generally speaking, patients in Africa want to be with their families and close to their ancestors at this time of life. The caring atmosphere is generally missing within hospitals in Malawi because they are so under-resourced - for example, you need to take a relative with you, otherwise there would be no-one to give you a wash or feed you.
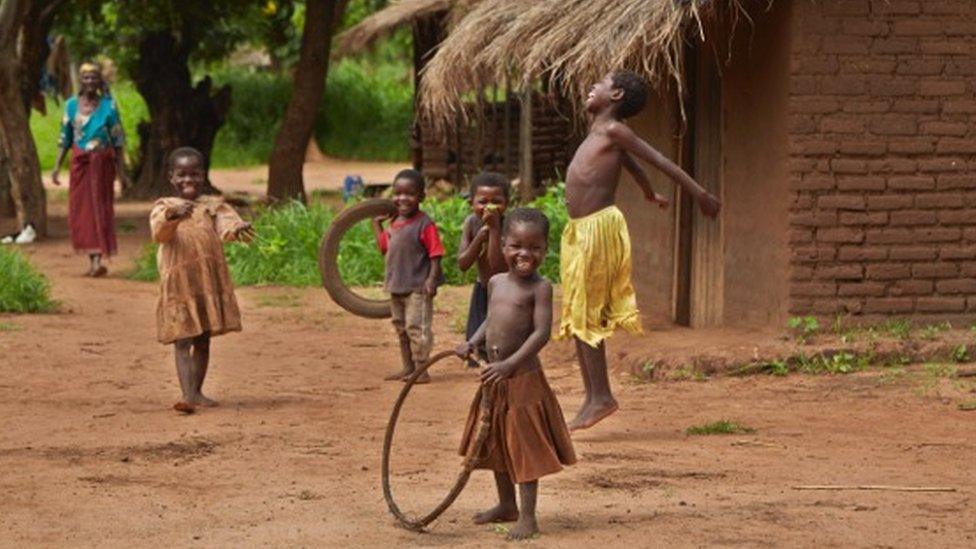
Providing palliative care at home means patients can remain in their community
It is important that palliative care starts at the point of diagnosis, not just as death becomes imminent. This provides an opportunity for the patient to deal with their fears about the future of those they leave behind, as well as fears for themselves.
These fears are entirely understandable because Malawi only has two oncologists for a population of nearly 17 million, and has no dedicated cancer centre. The available chemotherapy is largely palliative rather than curative.

What is 100 women?
BBC 100 Women names 100 influential and inspirational women around the world every year. We create documentaries, features and interviews about their lives, giving more space for stories that put women at the centre.
Other stories you might like:
'I married a man to keep my girlfriend'
'Adults are so obsessed with children they have no time for important things'

There is also lack of early diagnosis so by the time the patients come to us the cancer is already advanced and for them the only option is palliative care.
Some 50% of people in Africa do not see a health worker their entire lives. They may use herbal medicines and traditional healers which are cheaper than Western-trained health workers. For example, in Uganda there is one traditional healer to 450 people and one doctor to 20,000.

Jonathan was suffering from oesophageal cancer and HIV. The bottles contain morphine which is an affordable way for patients to manage their pain at home.

His family wait outside his hut
Our care is holistic, which means that our trained staff multi-task in the relief of social, psychological and spiritual pain, as well as physical, whereas in the West different professionals would deal with different aspects of care. We know that unless we deal with these other aspects of pain - the social, the psychological and the spiritual - the physical pain cannot be managed.

Ndi Moyo grows herbs as an affordable way to help their patients:
Lemon grass helps patients excrete toxins
Aloe is a good balm for wounds and acts as a useful laxative
Artemisia has powerful immunity-boosting properties
Papaya sap is useful as an antiseptic
Vinca rosa lowers the white blood cell count
Source: Ndi Moyo

Holistic and extended care offers the terminally ill the time to make peace with any with whom they have been in conflict, the chance to forgive and be forgiven, the chance to renew love and be loved.
I feel that sometimes in the West it is easier for a doctor to suggest another treatment to a patient rather than to have the more difficult conversation about whether it may be better not to continue to treat a serious illness, partly because expectations in the West are higher.
Holistic palliative care as practised here is not about adding days to life, but adding life to the days that remain.