Cancer in Senegal: 'I had to sell everything to pay for treatment'
- Published

Awa Florence, 50, fears she won't be able to get all the cancer treatment she needs
"It's really expensive. When all this started, I had to sell everything I owned," says cancer patient Awa Florence.
"I don't have anything left. I'm a widow and I don't have the means to pay for further tests."
The school administrator from Senegal's capital city, Dakar, was diagnosed with cervical cancer last year.
Cancer is a growing problem in Africa and Senegal is the latest country to try to improve patient care by subsiding chemotherapy in all public hospitals.
The government says the drugs will be free for women suffering from breast or cervical cancer and up to 60% cheaper for other types of cancers.
Some of the essential drugs needed to treat the side effects of chemotherapy will also be covered, Khady Mbaye Sylla, director of public hospitals, tells the BBC.
'Like new tyres'
But cancer often requires more complex treatment than just chemotherapy alone, and that costs more money, which patients have to pay for.
"It's a bit like getting new tyres. For your car to work, you still need to buy gas, to have roads, a driving licence," says Dr Ben Anderson, director of the Breast Health Global Initiative.

"When I first saw the invoice I started to cry," Ms Florence says
Cervical cancer and breast cancer are the biggest causes of cancer deaths among women in sub-Saharan Africa, according to the World Health Organization (WHO).
Yet it is only in recent years that prevention and control of these diseases have become a matter of public health.
In 2011, the WHO said that non-communicable diseases were "an impending disaster" for some countries, external, pushing millions of people into poverty.
So, Senegal's efforts should be lauded as "an excellent step", says Dr Anderson.

Cancer in Senegal:
Most common cancers: cervix (17.8); breast (16.7%); liver (10.2%); prostate (9.1%); stomach (5.2%)
Number of new registered cancer cases (2018): 10,549 - from a population of 16 million
Number of registered cancer deaths (2018): 7,571
Source: WHO, external

Until recently, healthcare for Africa's women has been designed primarily around acute, infectious diseases and pregnancy-related complications.
But with increases in life expectancy and also what doctors term "risky health behaviours" - poor diets, lack of exercise, using alcohol and tobacco - the burden of cancer has been rising on the continent.
One of the few oncologists working in Dakar tells the BBC that to effectively reduce cancer mortality, much more can and must be done.
"We need to subsidise cancer treatments entirely, from early detection to palliative care," says Dr Mamadou Diop.
In addition to chemotherapy, patients often need surgery, and some need hormonal therapy or radiotherapy.
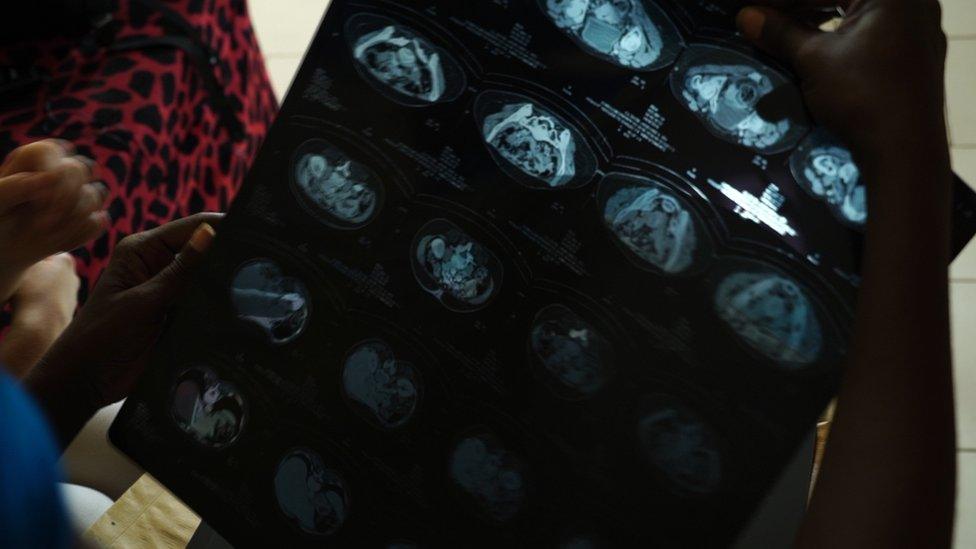
These are the scans which showed that Ms Florence has cancer
In Senegal, a course of radiotherapy can cost about $250 (£195) and surgery $330. That is after the patient has undergone required tests and examinations that can cost up to $1,600.
For women like Ms Florence, who earns about $80 a month, it is just too expensive.
Ms Florence is hopeful the new measure could help women like her, but also has some reservations.
"They say it's for free, but we don't know if we will need to fill out paperwork here and there, and if we need to buy drugs urgently…," she says, her voice trailing off.
"Will the government pay for radiotherapy that costs $250 or scans that cost $130? If the government pays all that, then yes - it's a good thing."
Lack of data
In the meantime, she has sought help for her medical bills elsewhere.
"When I first saw the invoice I started to cry. I told my doctor I couldn't pay it and he put me in touch with the Anti-Cancer League who were able to help me."
"I have an appointment soon for radiotherapy and I'll bring the results to the doctor who will tell me what to do next," Ms Florence says.
"Chemotherapy is really hard. I would prefer him to tell me I don't need to do it again… The side effects are painful and you're supposed to eat healthy food, fruits, but it's hard when you don't have the means."

Senegal's Anti-Cancer League organises free cancer screening days
Despite the announcement from Senegal's government, Dr Diop believes there are still many cancer sufferers across the country who aren't receiving any treatment at all, with many people not knowing they have it.
Overall the five-year survival rate across different cancers is as low as 10 to 20% in low-income countries, while in richer countries it averages between 80 and 90%, says Dr Prebo Barango of the WHO.
Factors include:
lack of information about early signs and symptoms of cancer
late diagnosis or misdiagnosis
weak or non-existent referral systems
geographical distance from care and treatment
catastrophic costs of treatment and medicines
weak healthcare systems and instances of abandoned treatment.
(Source: WHO)
A key challenge across many African countries, however, is the severe lack of data when it comes to cancer prevalence. This makes it harder for policy-makers to assess and act upon.
Why some Africans believe they'll get better healthcare in India
Dr Barango says about a third of all cancer cases could be prevented by avoiding key risk factors.
Most African nations have "stepped up prevention of cancer risk factors", he says, implementing tobacco control programmes for example.
Efforts are being made to widen access to cervical cancer screening and pre-cancer treatment in cost-effective ways, Dr Barango adds.
Cervical cancer is the most common form in Africa yet can be largely prevented through vaccination and screening, according to the WHO.
Numerous countries - among them Botswana, South Africa, Zimbabwe, Senegal, Ethiopia and Malawi - have introduced the HPV vaccine to help prevent cervical cancer into their national immunisation programmes.
As it stands, most cancer patients in Africa are diagnosed at a late stage and the prognosis for a positive outcome is reduced - even in cases where treatment is available and affordable, says the WHO's African regional director Dr Matshidiso Moeti.
If more money were spent raising public awareness on the early signs of common cancers - and urging people to adopt healthier lifestyles - experts believe that many more lives would be saved.
- Published25 November 2019

- Published13 February 2019

- Published19 June 2019

- Published1 August 2019

- Published25 February 2019

- Published9 July 2024
