Coronavirus in Africa: Contained or unrecorded?
- Published

The World Health Organization (WHO) has warned that nearly a quarter of a billion Africans could contract coronavirus in the first year of the pandemic, with between 150,000 and 190,000 of them dying.
Africa has had less than 100,000 cases so far, but WHO experts believe the continent will have a prolonged outbreak over a few years - and, aid workers say, the huge focus on containing the virus has led to other health issues being neglected.
Here, five BBC reporters give a snapshot of what is happening in their countries:

Congolese 'probably had virus without knowing it'
By Emery Makumeno, Kinshasa

DR Congo is grappling with coronavirus and Ebola
The Democratic Republic of Congo confirmed its first case of Covid-19 in early March, but a doctor in the capital, Kinshasa, believes the disease arrived earlier.
"During December and January, I can't remember how many patients came for medical treatment, coughing and with fever and headaches," he said, referring to Covid-19 symptoms listed by the WHO.
"I am convinced that we, the medical staff, have been exposed to coronavirus already, without knowing it, and we have built a sort of immunity," he added.
But DR Congo has carried out few tests to check the Covid-19 status of people, because of a lack of medical equipment.
Countries with successful testing strategies, external, such as South Korea and Germany, have rapidly reached at least 1% of their population, UK medical journal The Lancet points out.
If equipment is available, many African states could ramp up tests - some, though not DR Congo, did more HIV tests between 1 October and 31 December than the 1% target for Covid-19 testing, The Lancet says.

Number of Covid-19 tests done in DR Congo by 18 May: 4,493
Tests required to make up 1% of population: 895,614
HIV tests done from 1 October to 31 December 2019: 203,859
Sources: Africa CDC; The Lancet

So far, DR Congo has recorded more than 1,600 cases of the virus - the ninth-highest number in Africa, according to WHO.
The first Covid-19 case was detected in La Gombe, the main business district in Kinshasa. The government moved swiftly to introduce a lockdown, but the virus has since spread to seven of the country's 26 provinces - including the mining hub of Lubumbashi.
The outbreak comes at a time when DR Congo - which has poor health services, and has been hit by decades of conflict in the east - is also grappling with an Ebola outbreak. It has killed more than 2,000 people since 2018. Covid-19 has so far claimed the lives of more than 60 people.
The UN children's agency, Unicef, has also raised concern about a reduction in vaccination rates, saying gains made from immunisation over the past two years could be erased.

Hundreds of thousands of children have not been vaccinated
Unicef said vaccinations were already declining at the beginning of this year, and that the effects of coronavirus will make it worse.
Hundreds of thousands of children had not received polio, measles, yellow fever and other vaccines.
DR Congo might lose its polio-free status and there could be a resurgence of other deadly diseases.
Health workers lacked equipment to protect themselves or the children from Covid-19, and parents were afraid to bring them to vaccination centres.

Kenya hospital has 'fewer patients but more corpses'
By Mercy Juma, Nairobi
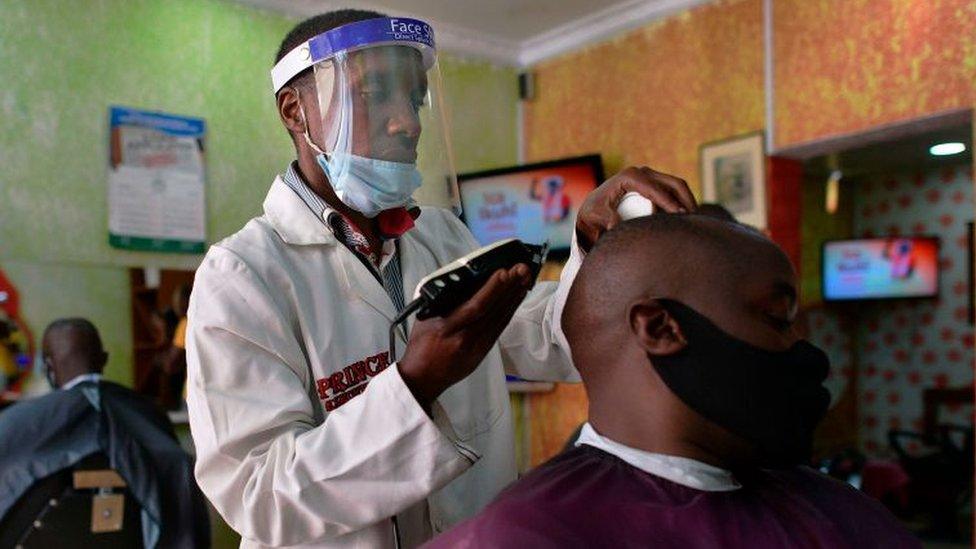
To cover your face become the norm in Kenya
A major public hospital in Kenya's capital, Nairobi, saw an almost 40% increase in respiratory illnesses such as tuberculosis, pneumonia and asthma between December and early March, a doctor who works there told the BBC.
However, the hospital had a sharp decline in such cases since mid-March, said the doctor, who spoke to the BBC on condition of anonymity as he was not authorised to speak to the media.
One reason was that the government had imposed a nationwide dusk-to-dawn curfew to contain the spread of coronavirus.
This has resulted in a drop in night-time admissions, but an increase in the number of dead people being brought to the hospital's mortuary, the doctor said.
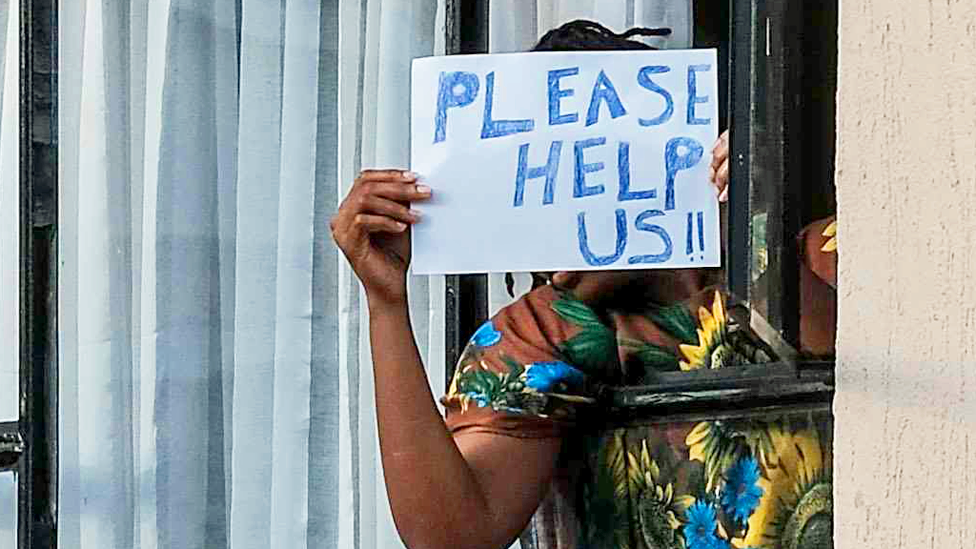
Some people have been desperate to get out of quarantine
People also seemed to be avoiding hospital for fear of being diagnosed with Covid-19 and being sent to quarantine centres, he said.
This is because quarantining has been controversial in Kenya, with the government forcing suspected Covid-19 patients to pay for their own confinement.
The price ranges from $20 (£16) to $100 a night, depending on the centre, though the government has now promised to cover costs at public quarantine centres.

Number of Covid-19 tests done in Kenya by 18 May: 44,851
Tests required to make up 1% of population: 537,713
HIV tests done from 1 October to 31 December 2019: 2, 177,170
Sources: Africa CDC; The Lancet

Hostels at schools and universities as well as private hotels have been used as quarantine centres.
A video clip went viral last month, showing several people scaling a wall to flee a centre in Nairobi.
Allow X content?
This article contains content provided by X. We ask for your permission before anything is loaded, as they may be using cookies and other technologies. You may want to read X’s cookie policy, external and privacy policy, external before accepting. To view this content choose ‘accept and continue’.

Those quarantined have complained that some centres are not much better than prisons, with poor hygiene and overcrowding making it impossible to practise social distancing.

'More patients and more corpses' in northern Nigeria
By Ishaq Khalid, Abuja

Very little testing for Covid-19 has been done in Nigeria
There have been reports of more people falling ill and dying in Nigeria's most populous state, Kano, since the outbreak of coronavirus nearly three months ago.
So, it is not surprising that President Muhammadu Buhari has extended the lockdown in the northern state to the end of the month.
A grave digger at the Abattoir Graveyard in the main city, also known as Kano, told the BBC: "We have never seen this, since the major cholera outbreak that our parents tell us about. That was about 60 years ago."
Prof Musa Baba-Shani - the head of the department of medicines at Aminu Kano Teaching Hospital, the main hospital in the state - told the BBC that they have been treating more patients with illnesses such as asthma, pneumonia, and tuberculosis, as well as chest pains and sore throats.
The professor, who works with the respiratory diseases unit of the hospital, said there had been an increase of between 40% and 45% in the number of respiratory cases in about the last three months.

Social distancing is often difficult in Nigeria
He attributed the rise to the closure of many hospitals in the state, especially private clinics, because of a lack of protective gear for medics. This has forced more patients to seek treatment at the Aminu Kano Teaching Hospital.
Prof Baba-Shani said some of those with respiratory illnesses were diagnosed with coronavirus, and referred to the treatment centres set up for Covid-19 patients.
He decried the slow testing for coronavirus in Africa's most-populous country, which has a population of around 200 million. It would be better for both patients and hospitals if testing was speeded up, he said.

Number of Covid-19 tests done in Nigeria by 18 May: 33,970
Tests required to make up 1% of population: 2,061,396
HIV tests done from 1 October to 31 December 2019: 1,160,920
Sources: Africa CDC; The Lancet

Another doctor at the hospital, who asked not to be named because he was not authorised to speak to the media, said some people were avoiding seeking treatment because they feared contracting Covid-19 in hospitals.
In north-eastern Yobe state, an unusually high number of people - 471 - have died in the past five weeks.
It is unclear whether the deaths are linked to coronavirus, but the state's health commissioner, Dr Muhammad Lawan Gana, told the BBC that a preliminary investigation had found that most of the dead were elderly people with pre-existing health conditions such as hypertension and diabetes.
Coronavirus in Nigeria: The engineers fixing ventilators for free
Nigeria has more than 6,000 confirmed cases of coronavirus, the third-highest in Africa.
The commercial capital, Lagos, is at the epicentre of the outbreak, but a lockdown imposed at the end of March has been partially eased, raising fears that the virus could spread.
"It's tough decision, but I think it was the wrong call," said Dr Andrew Iroemeh, who works at a Covid-19 isolation centre in the city,
"It's recommended [that] for a lockdown to be relaxed we should have a consistent reduction in the rate of infection for at least 14 days. We haven't seen that," he added.

'Few signs of virus' in Ethiopia
By Kalkidan Yibelta, Addis Ababa

Ethiopia has banned gatherings of more than four
Respiratory infections are common in Ethiopia, Africa's second most-populous state, with a population of more than 100 million. Research shows they are the third major cause of death each year, after neonatal disorders and diarrheal diseases.
The coronavirus outbreak does not seem to have led to more patients with respiratory infections being admitted to hospitals over the past few weeks.
A doctor in the capital, Addis Ababa, told the BBC that he was looking for signs of unreported Covid-19 cases but he did not detect anything unusual.

Number of Covid-19 tests done in Ethiopia by 18 May: 59,029
Tests required to make up 1% of population: 1,149,636
HIV tests done from 1 October to 31 December 2019: 136,307
Sources: Africa CDC; The Lancet

There was no increase, for example, in the number of patients with pneumonia, a severe complication caused by the virus.
Similar reports were given by a doctor and a nurse the BBC spoke to in eastern and southern Ethiopia respectively.
In recent days, the number of cases detected daily has risen from single to double digits. This has raised some concern, but the overall number is still low - less than 400.
This is despite the fact that Ethiopia, unlike many other states, has not introduced a lockdown, taking limited measures, such as a ban on sporting events and gatherings of more than four people, to curb the spread of the virus.
Coronavirus: Ethiopian pop star donates house to help fight virus
The doctor in Addis Ababa said Ethiopians might have been spared the worst of the virus because of less foreign travel, or there may be other unknown factors at play.
He said people should take precautions to prevent the spread of the virus as the possibility of a surge could not be ruled out.

Uganda to focus on 'verbal autopsies'
By Catherine Byaruhanga, Kampala

Traders have been ordered to sleep in markets to reduce the risk of them taking the virus to their homes
Uganda has imposed one of the strictest lockdowns in East Africa and so far it has one of the lowest number of Covid-19 cases in the region - around 260 - and no deaths.
Most of the testing in Uganda has been on truck drivers who arrive from neighbouring states. Last week, Health Minister Ruth Aceng said that of the 139 confirmed cases at the time, 79 were truck drivers.
The President of the Uganda Medical Association, Dr Richard Idro, said that doctors around the country had not reported seeing more patients with respiratory illnesses, though the lockdown - which includes a ban on travel - could have prevented them from going to hospital.
People with mild symptoms of coronavirus might have also stayed at home, resulting in some cases going unrecorded.

Number of Covid-19 tests done in Uganda by 18 May: 87,832
Tests required to make up 1% of population: 457,410
HIV tests done from 1 October to 31 December 2019: 2,098,734
Sources: Ugandan government; The Lancet

In a recent address, Uganda's President Museveni said the government planned to carry out "verbal autopsies" in communities to find out whether people might have died from Covid-19.
The government has promised to distribute free masks to all citizens above six years old over the next two weeks before easing lockdown measures.
Ugandans on social media have generally been sceptical about the plan, pointing to the delays in giving food to 1.5 million people in and around the capital, Kampala, after they lost their income because of Covid-19 restrictions.
If the mask distribution is successful, Mr Museveni has promised that shops will be allowed to open, public transport will be back on the road but carrying half the number of passengers and food market vendors - who have been sleeping at their stalls under the president's orders - will be allowed to go home at the end of each day.

GLOBAL SPREAD: Tracking the pandemic
RECOVERY: How long does it take to get better?
A SIMPLE GUIDE: What are the symptoms?

- Published18 May 2020

- Published12 May 2020

- Published17 May 2020

- Published13 May 2020
