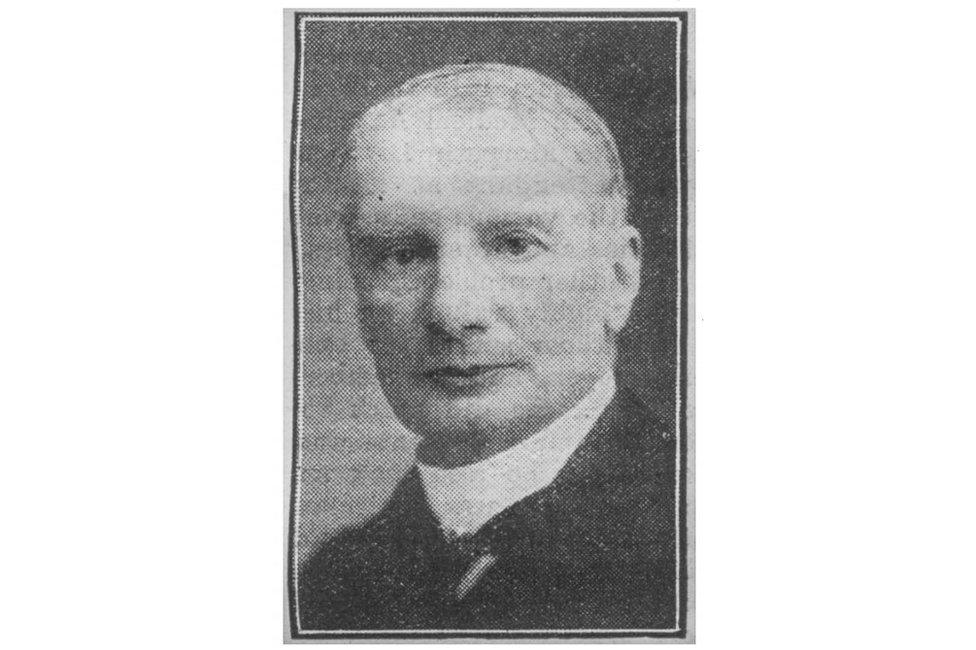
Waldemar Haffkine: The vaccine pioneer the world forgot
- Published

Working in Paris and India at the turn of the last century, Waldemar Mordecai Haffkine created the world's first vaccines for cholera and plague. Then an accidental mass poisoning derailed his life.



In the spring of 1894, Waldemar Haffkine travelled to Calcutta in the Indian province of Bengal in search of cholera. Spring was cholera season in the city, and Haffkine was hopeful.
He had arrived in India the previous March armed with what he believed was a vaccine for the disease, but he struggled all year to make progress testing his creation. From the moment of his arrival, Haffkine was met with scepticism and resistance from some of the British medical establishment and the Indian public. He was not a doctor but a zoologist. And he was a Russian Jew who had trained in Odessa and developed his skills in Paris, at a time when the world of international bacteriology was factional and prone to suspicion.
Haffkine, who was 33 when he landed in India, also struggled with the practical side of testing his vaccine. His first iteration required two injections, separated by a week, and his team sometimes struggled to locate test subjects for the second prick. And despite the wide spread of cholera in India, finding it in sufficient concentration wasn't straightforward. Haffkine inoculated about 23,000 people that year in northern India, according to his own records, "but no cholera appeared in their midst to show whether the vaccine was of value or not".
Then in March 1894, Haffkine got a break. He was invited to Calcutta by the medical officer there to help identify cholera bacilli in a water tank in one of the city's bustees - isolated villages on the outskirts of the city consisting of mud huts clustered around ponds or tanks and inhabited by the city's poor. The families living in these bustees drank collectively from the shared water sources, making them vulnerable to periodic outbreaks of cholera.

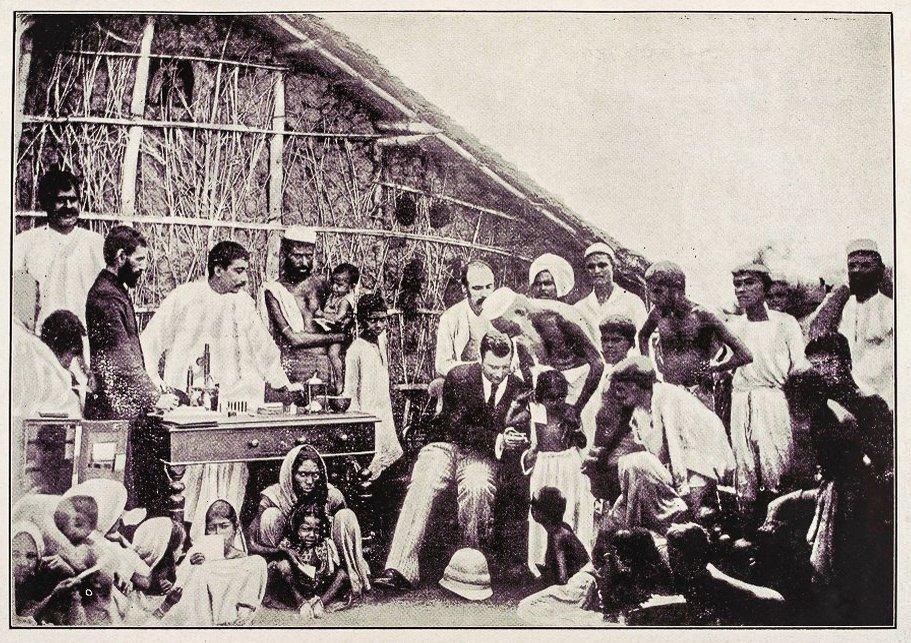
Haffkine inoculating villagers in Calcutta in March 1894

To Haffkine, the bustees were an ideal proving ground for his nascent vaccine. In each household, he had a group of people living in identical conditions, equally exposed to cholera. If he could inoculate some of each family and leave some untreated, with enough participants he might finally produce some meaningful results.
At the end of March, two people died of cholera in the Kattal Bagan bustee, signalling a new outbreak. Haffkine travelled to the bustee and inoculated 116 of the 200 or so inhabitants. Afterwards, his small team observed 10 further cases there, seven fatal - all among the uninoculated.
The results were encouraging enough for the Calcutta health officer to fund a wider trial, but convincing people to be vaccinated was easier said than done. Years of top-down medical programmes by the British government had sowed distrust among the population, and to many the very concept of vaccination was still alien.
Haffkine's solution was to work with a team of Indian doctors and assistants, rather than the British - Drs Chowdry, Ghose, Chatterjee, and Dutt, among others. And he had a new trick up his sleeve in the world of vaccinology: publicly injecting himself to prove he thought his preparation was safe.

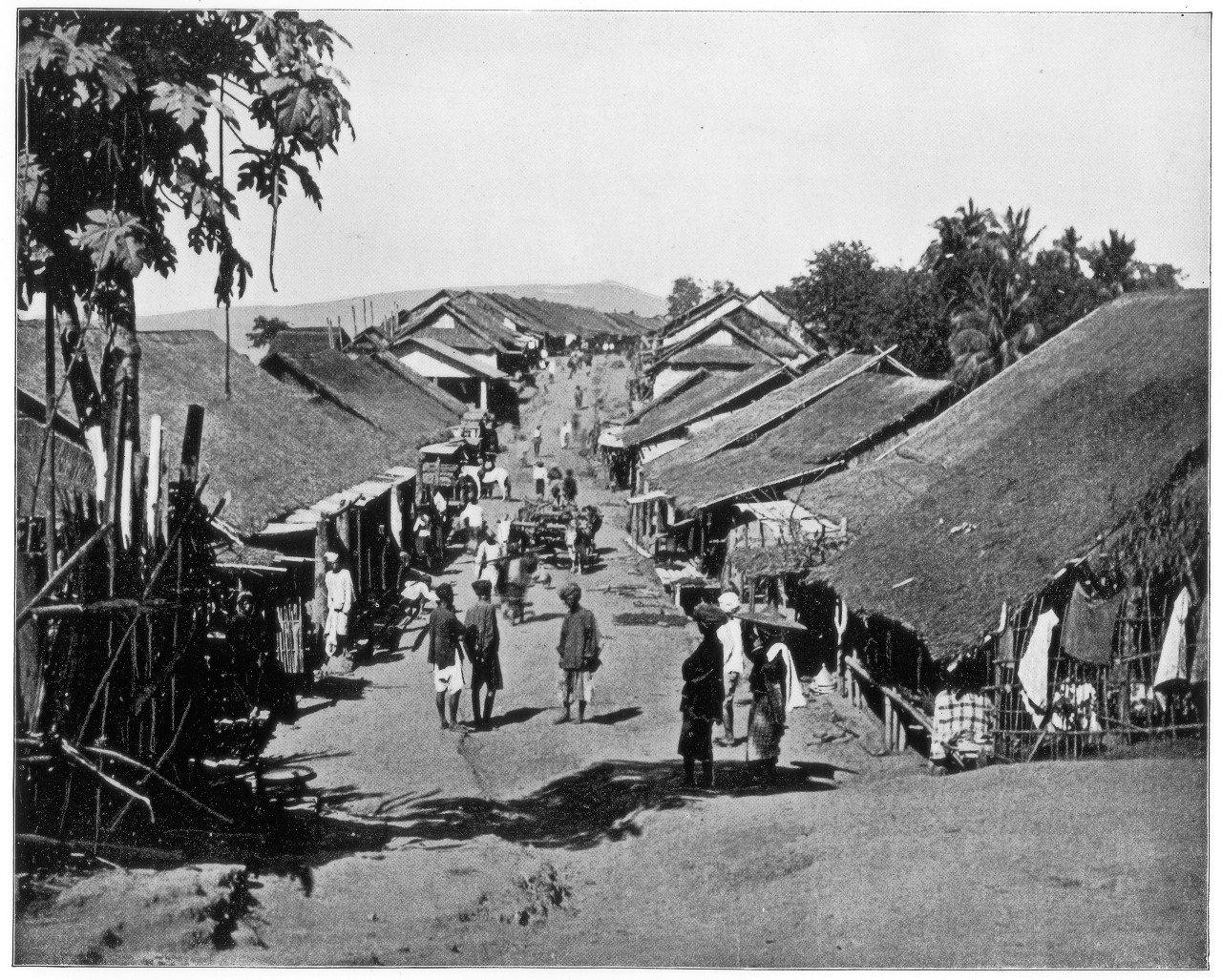
Cholera spread easily through villages like this one in Calcutta, pictured in the 1890s

"What is remarkable, and is often lost in the story, is that after the initial resistance people began to queue in the slums in Calcutta for Haffkine's cholera vaccine, they queued for the whole day," said Professor Pratik Chakrabarti, the Chair in History of Science and Medicine at the University of Manchester.
"He would spend hours and whole days in those slums working with Indian doctors. He would start vaccinating in the morning before people went to work, and continue after they came back in the evenings, sitting by an oil lamp in the slum."
Haffkine's work in the Calcutta slums placed him among a select group of scientists who pioneered a profound and global shift in the way disease was understood and treated. But unlike Edward Jenner before him and Jonas Salk after, Haffkine's name never really entered the public imagination, either in India or in Europe.
"Haffkine was the first person who brought that kind of laboratory medicine into a tropical country like India," Professor Chakrabarti said.
"He was a Paris scientist who came to the slums of Calcutta. He has a very dramatic story."

When Haffkine graduated in zoology from the University of Odessa in 1884, his reward was to be barred from taking up a professorship there because he was a Jew. He had already run into political trouble five years earlier, amid pogroms, when as a member of a local defence league he fought to stop Russian army cadets destroying a Jewish man's home. Haffkine was beaten and arrested but eventually released.
In 1888, Haffkine left his home country and found his way first to a short-lived teaching job in Geneva and then to Paris, where he took a position as an assistant librarian at the Louis Pasteur institute - then the world's leading centre of bacteriology research. In his free time from the library, Haffkine either played the violin or experimented in the bacteriology lab.
Building on the work of Pasteur and Jenner, Haffkine discovered that by passing cholera bacilli through the peritoneal cavity of guinea pigs - 39 passes in total - he could produce a strengthened, or "exalted" cholera culture, which he could then attenuate using heat. An injection of the attenuated bacteria, followed later by an injection of the exalted bacteria, appeared to immunise guinea pigs against a lethal attack of the disease.
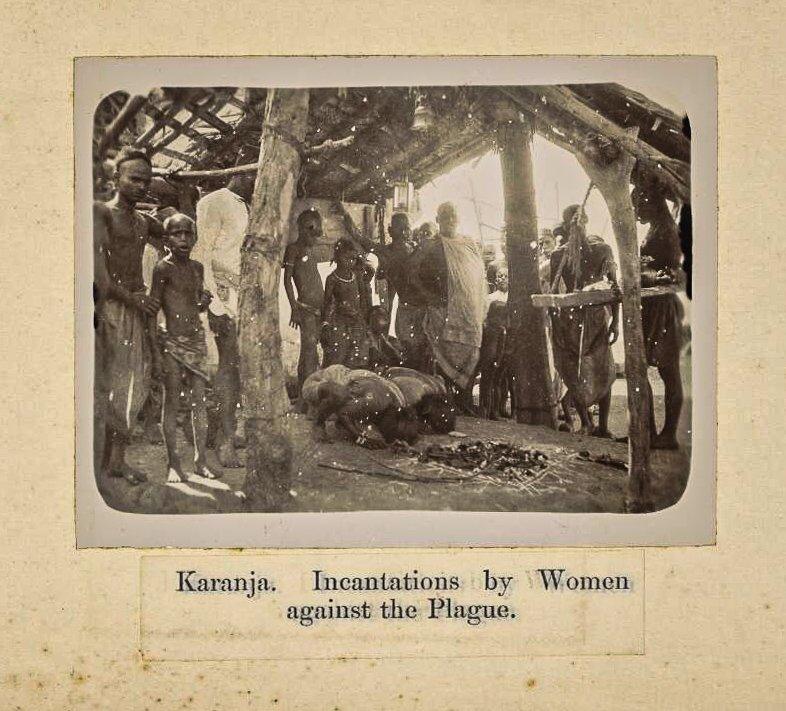
Up until that point, diseases like cholera had been thought of in miasmatic terms - that they travelled in bad air - and tackled with what Professor Chakrabarti called "broad spectrum treatments". ("You put someone in a bath and steam them until they are half dead, or spray carbolic acid everywhere.") But the work of Haffkine and others was giving disease management a focal point - a virus or bacterium that could be cultivated and attenuated, targeted precisely in the body.

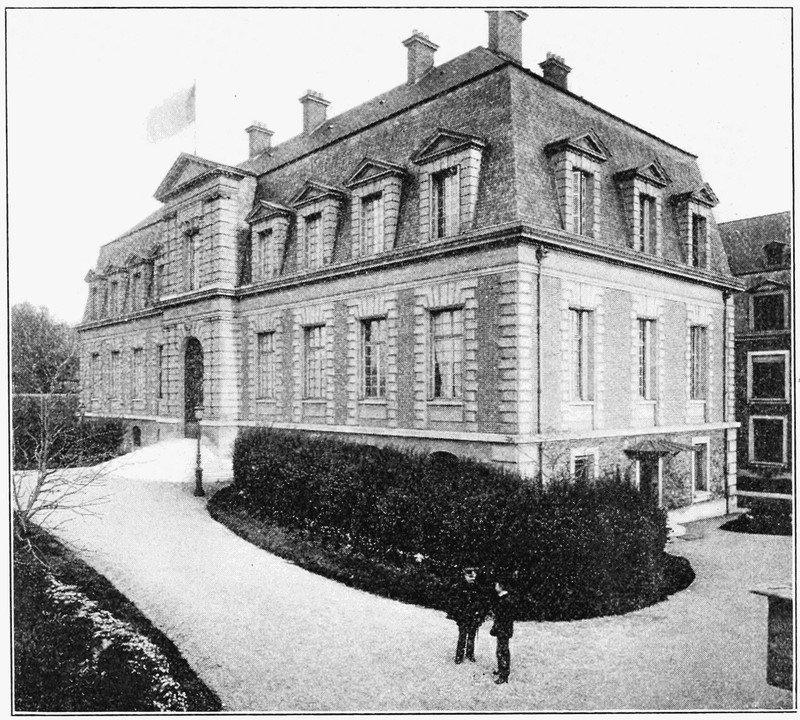
The Pasteur Institute, Paris, where Haffkine developed his cholera vaccine in 1892

A week after his success with guinea pigs in Paris, Haffkine replicated the results with rabbits and then pigeons. He was ready for a human.
On 18 July 1892, Haffkine risked his life by injecting himself with attenuated cholera. He suffered a fever for several days but recovered fully, and went on to inoculate three Russian friends and then several other volunteers. When each suffered no worse reaction, Haffkine was convinced he had a viable vaccine for wider testing.
But he needed somewhere rife with cholera to conduct large human trials. In 1893, Lord Frederick Dufferin, then the British ambassador in Paris and a former Viceroy of India, heard of Haffkine's situation and suggested he go to Bengal.
After Haffkine's experiments in the bustees of Calcutta the following year yielded promising results, he was invited by the owners of tea plantations in Assam to vaccinate their workers. Haffkine conducted large scale trials there on thousands of plantation workers, but in the autumn of 1895 he contracted malaria and was forced to return to England to recuperate. According to his records, he had by that point inoculated nearly 42,000 people against cholera.
Haffkine noted later that while his vaccine appeared to reduce cases, it did not appear to reduce mortality in those who were infected. When he returned to India in 1896, he planned to address this deficiency by testing a new two-pronged formula he had developed. But there was a more pressing problem in Bombay that would take Haffkine away from cholera for good.

The world's third plague pandemic began in Yunnan, China in 1894. It spread down to British Hong Kong and from there by merchant ship to the bustling coastal metropolis of Bombay in what was then British India, where the first case was discovered in September 1896 at a grain merchant's quarters at the city's docks.
At first, the British government underplayed the severity of the outbreak, keen to keep a key port city open for business. But the disease tore through Bombay's tightly-packed slums - its mortality rate nearly twice that of cholera - and the number of dead soared. The governor turned to Haffkine for help. Haffkine travelled to Bombay, where he was set up in one small room and a corridor, with one clerk and three untrained assistants, and tasked with coming up with the world's first plague vaccine from scratch.
"He didn't have a lot in terms of space, manpower or facilities, but it was the first time he was working independently and had his own lab," said Chandrakant Lahariya, an epidemiologist in Delhi. "He knew that developing a plague vaccine at record pace would make him a leading scientist of his time."

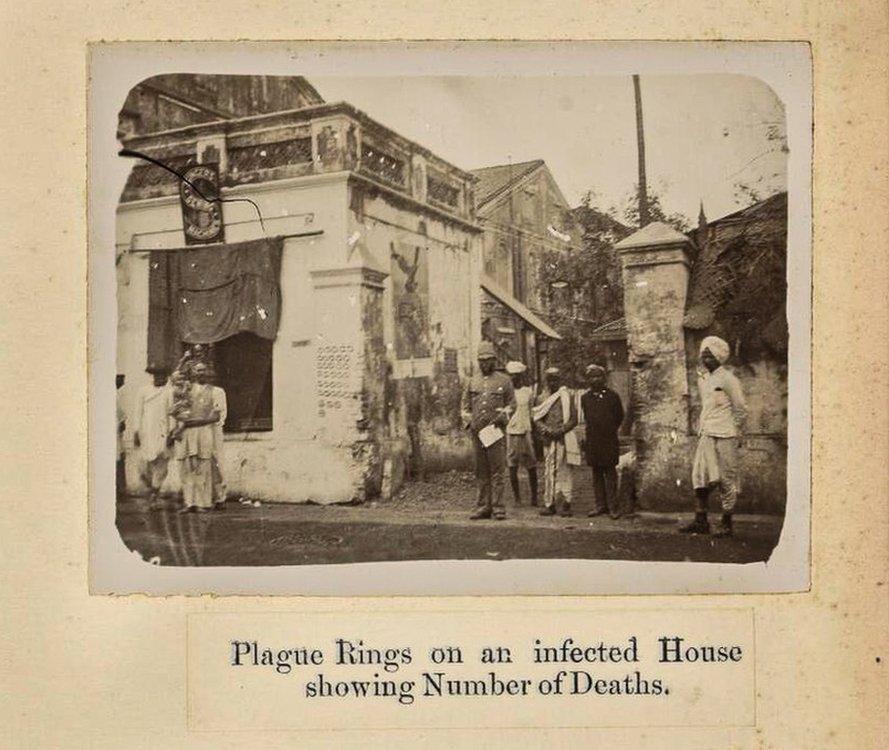
Rings chalked on a Bombay home, showing the number of plague cases within

Haffkine worked tirelessly through that winter. He discovered that if he placed plague bacilli in a nutrient broth to which he had added a small quantity of clarified butter or coconut oil, the bacilli formed into a signature stalactite growth, creating microbes and toxic products on the side. He was using the same approach he had devised for the new treatment of cholera, combining the microbes with the toxic products they produced to form a single-injection vaccine.
In December, Haffkine successfully inoculated rabbits against an attack of plague, and by January 1897 he was ready once again to test a fresh vaccine for a deadly disease on a human.
On 10 January 1897, Haffkine injected himself with 10cc of his preparation - a significantly higher dose than the 3cc he planned to use in wider testing. He experienced a severe fever but recovered after several days.
At the end of that month, a plague outbreak occurred at Bombay's Byculla House of Correction - a jail housing hundreds of inmates - and Haffkine went there to carry out controlled tests. He inoculated 147 prisoners and left 172 untreated. There were 12 cases and six deaths among the untreated and just two cases and no deaths among the treated.

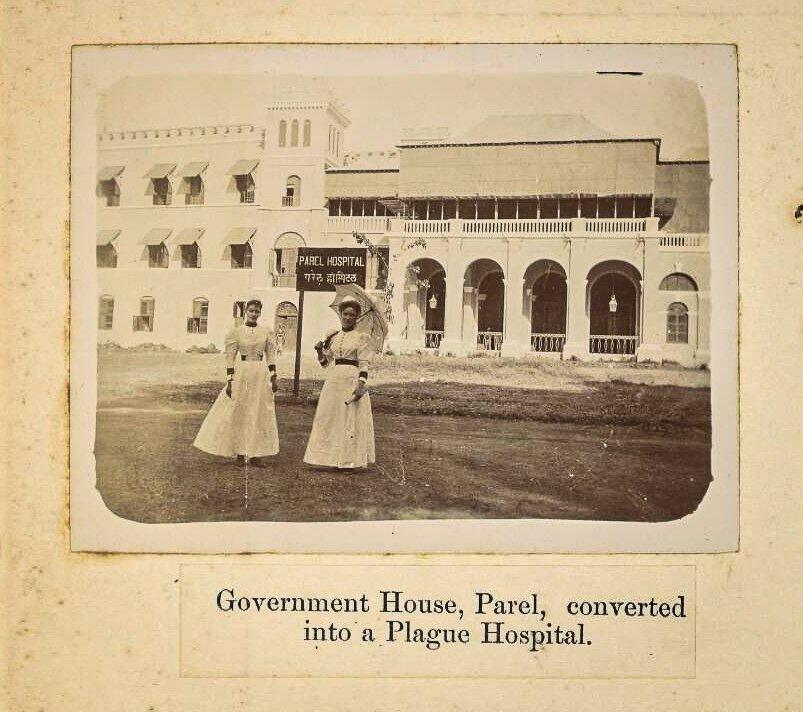
Haffkine was set up in new offices at what became known as the 'Parel lab'

The apparent success at Byculla jail set off a rapid expansion of production and testing and Haffkine was relocated from his small one-room laboratory to a government-owned bungalow, and then on to a large lodge owned by the spiritual leader the Aga Khan, who also volunteered himself and thousands of members of his Khoja Mussulman community for inoculation.
Inside a year, hundreds of thousands of people had been inoculated using Haffkine's vaccine, saving untold numbers of lives. He was knighted by Queen Victoria, and in December 1901 he was appointed director-in-chief of the Plague Research Laboratory at Government House in Parel, Bombay, with new facilities and a staff of 53.
Then disaster struck.
In March 1902, in the village of Mulkowal in Punjab, 19 people died from tetanus after being inoculated with Haffkine's vaccine. The 88 others inoculated that day were fine. All the evidence appeared to point to a fatal contamination of bottle 53N - prepared 41 days earlier at the Parel lab.
An Indian government commission was tasked with investigating, and it discovered that Haffkine had changed the procedure for sterilising the plague vaccine, using heat instead of carbolic acid because it sped up production. The heat method had been safely in use at the world-leading Pasteur institute for two years, but it was unfamiliar to the British, and in 1903 the commission concluded that bottle 53N must have been contaminated in Haffkine's lab in Parel. Haffkine was fired as director of the plague lab and placed on leave from the Indian Civil Service.

Disgraced by the verdict, Haffkine left India and travelled to London. He had developed a plague vaccine at heroic speed and been knighted by the Queen, but suddenly he found himself on the outside. It was a position to which he was not entirely unfamiliar.
"There was a lot of bias in those days, a lot of prejudice," said Dr Barbara Hawgood, a lecturer who published an academic paper on Haffkine's career. "He wasn't medical, so he wasn't one of them. There was a lot of arrogance about that."
Eli Chernin, a Harvard professor of public health who studied Haffkine's correspondence, wrote that it "was not evident from the archives that Haffkine was overtly victimized by anti-Semitism", but it "would be naive to think that the Edwardian bureaucracy was wholly uninfluenced by Haffkine's being a Jew".
And Haffkine faced smaller, more private battles, according to Chernin - struggling to express himself easily in English. Behind the letters he wrote during this time, even to his friends, there were drafts that were "almost undecipherable masses of scrawls, interlinings, and crossings-out, all later carefully transcribed".



In 1904, two years after Haffkine was suspended, the plague reached its peak in India, killing 1,143,993 people that year. Haffkine's vaccine was the "main line of defence", Dr Hawgood said, but its creator was stuck in London fighting for his name.
Four years after Mulkowal, in 1906, the Indian government finally published its full inquiry finding Haffkine guilty. Upon reading the masses of documents, WJ Simpson, a professor at King's College, London, wrote a letter to the British Medical Journal arguing passionately that the evidence pointed to an accidental contamination of bottle 53N at the inoculation site in Punjab.
First, there was no smell recorded from the bottle when it was opened, whereas a developed culture of tetanus would have produced a foul and distinct odour, he wrote.
Second, when the bottle was examined 15 days later there was only a poor culture of tetanus there. "If the bottle had been contaminated in Bombay," the commission "would have found in the dregs of the bottle a rich instead of a poor culture," Simpson wrote.
Third, the tetanus developed slowly in the 19 people who died, over seven to 10 days, indicating a weak infection beginning on the day of inoculation. With a well-developed culture already in the bottle, they "would have been attacked by a tetanus of the fulminating variety".

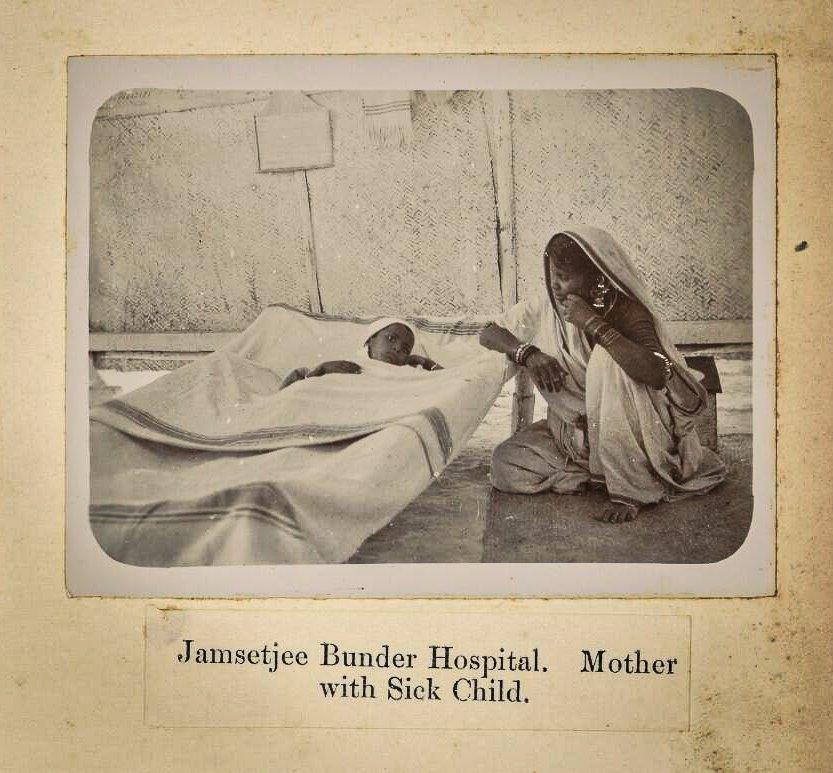
A mother with a child sick from plague in Bombay

Perhaps most importantly, the documents revealed that the assistant who opened bottle 53N dropped his forceps on the ground and failed to sterilise them properly before using them to remove the bottle's cork stopper.
Haffkine had been subjected to a "grave injustice", Simpson concluded. After his letter was published, others took up Haffkine's cause. In four scathing letters to The Times ("hot letters", he called them), the Nobel laureate Ronald Ross accused the British of "disregard for science" and warned that unless the decision against Haffkine was overturned, the government of India would be guilty of a "gross ingratitude to one of its greatest benefactors".
Ross also issued another warning, one which resonates today - that if the conclusion were allowed to stand that bottle 53N was contaminated in the lab, it threatened to undermine public trust in vaccines at a time when at least 50,000 people were dying every week from plague.


Haffkine was finally exonerated in November 1907, after Simpson and Ross's campaign raised the matter in the British parliament. Haffkine was granted leave to return to employment in India and he gladly returned as director in chief of the Calcutta Biological Laboratory. But his redemption was incomplete - he was barred from carrying out any trials, limiting him to theoretical research. "The whole of the unjust punishment for Mulkowal has been placed and remains on me quite as before," he wrote in a forlorn letter to Ross. "On every occasion in print and in speech it is repeated and kept alive that I was and am responsible for the case."
The following seven years were a fallow period for Haffkine. Of the 30 papers he produced in his lifetime, only one was published between 1907 and 1914. He returned briefly to the study of cholera and became interested in developing a new "devitalized" vaccine - a method that would later become widely used - but his repeated applications to the Indian government to carry out trials were refused. In 1914, aged 55, Haffkine retired from the Indian Civil Service and left the country. The Mulkowal disaster had been indelibly printed on him, and done him lasting damage.


"Mulkowal is his end story," said Pratik Chakrabarti. "It colours his legacy. He left India dejected and he is not a public figure. He has been lost to history."
Haffkine "should be much more well known," said Barbara Hawgood. "He really was a very good bacteriologist."
Between 1897 and 1925, 26 million doses of Haffkine's anti-plague vaccine were sent out from Bombay. Tests of the vaccine's efficacy showed between a 50% and 85% reduction in mortality. But "no figure" could be put on the number of lives he saved, Dr Hawgood said. "The numbers are just enormous."
Haffkine returned to France and devoted his later life to his faith, becoming increasingly orthodox and establishing a foundation to promote Jewish education in Eastern Europe. He never married and lived his final years alone in Lausanne, Switzerland. He was a "scholarly, lonesome, handsome man of few words, who remained a bachelor," wrote the Indian bacteriologist HI Jhala.

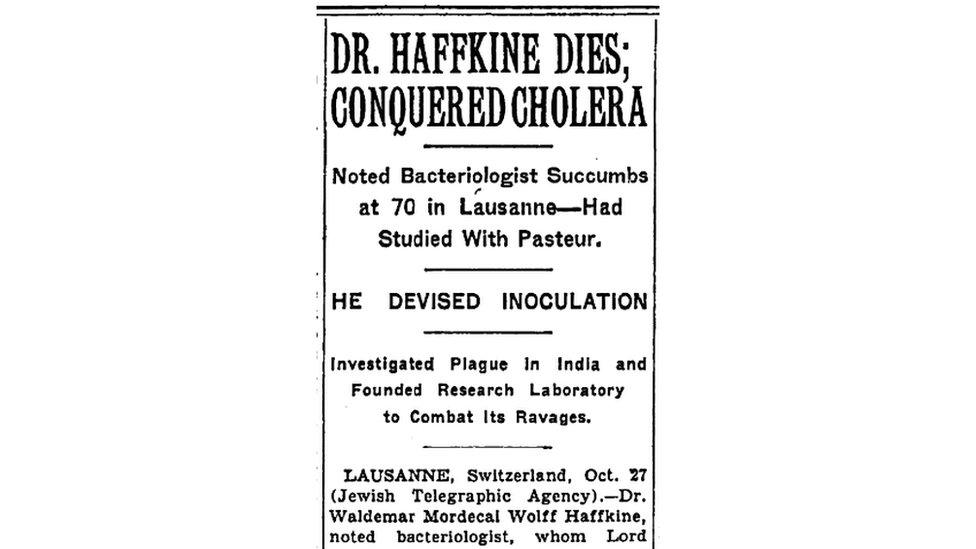

Haffkine died in Lausanne in 1930, aged 70. A short obituary notice circulated by the Jewish Telegraphic Agency noted that his plague vaccine had been "adopted throughout India" and his lab had "issued many thousands of doses to various tropical countries". The notice also quoted Lord Lister, the great British bacteriologist and pioneer of antiseptic surgery, who called Haffkine, simply, "the saviour of mankind".
The two-room lab where Haffkine first developed his plague vaccine is now part of the Grant Medical College and Sir JJ Group of Hospitals, Mumbai. More than a hundred years after Haffkine's breakthrough there, the hospital is playing a role in India's fight against another pandemic - the novel coronavirus.
"He inspired so many scientists to take up vaccine research in the early 20th Century, but somehow his contributions were forgotten," Dr Lahariya said. "We should never forget that Haffkine made a viable vaccine in a two-room lab with a very small team. It is almost unbelievable."
Haffkine's name does live on prominently in one sense. In 1925, five years before his death, the Indian government was lobbied by some of his supporters to rename the Parel lab 'The Haffkine Institute'. The government agreed, and the name remains to this day.
When Haffkine received a letter notifying him of the change, he wrote back to then-lab director Lieutenant-Colonel Mackie and his team, displaying no trace of bitterness from the many years spent in the shadow of Mulkowal.
"I am very greatly indebted to Col Mackie for the name given to the Parel Laboratory," Haffkine wrote.
"The work at Bombay absorbed the best years of my life and I need not explain how much I feel everything connected therewith. I wish the Institute prosperity as an active centre of work on behalf of the health organisation of the country, and I send blessings to the whole of its staff."
