Signing up to cervical cancer trial was 'easy decision'
- Published
Tara Millar signed up to a drugs trial for cervical cancer.
The first woman to take part in a cervical cancer trial in Northern Ireland has said signing up to it was a "no brainer".
The trial, which targets women who are too late to undergo surgery, gives six weeks of additional chemotherapy.
On average, 94 women in Northern Ireland each year are diagnosed with cervical cancer. Approximately 22 will die.
Tara Millar from Belfast was diagnosed on 1 April 2015.
After her diagnosis which was stage 2b, research staff at the cancer centre in Belfast offered her the choice of joining the UK trial.
"After I did all the research it was a no brainer," she said.
"I knew I was going to lose my hair and I had a mane of hair at the time. In fact, it weighed four pounds when it was cut off.
"But I looked at the facts and it gave me a higher percentage chance of surviving. "
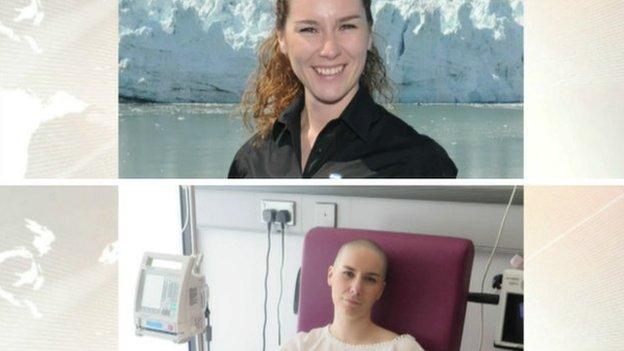
Tara Millar, before and after being diagnosed with cervical cancer
The trial, which is called Interlace, is being conducted by Cancer Research UK. This week it awarded £1.3m to Belfast Experimental Cancer Medicine Centre for trials.
Currently, four women in Northern Ireland are taking part in the trial, which is now in phase three of its research.
Additional nurses are often required which offer one-to-one treatment to the patient.
Wendy Cunningham has been a cancer research nurse for 20 years and looked after Tara.

Tara Millar on her wedding day
"The trial involves half of the women getting two extra drugs (carboplatin and paclitaxel) for about six weeks before their standard round of chemotherapy starts," she said.
"And these drugs are already being used for ovarian and breast cancer. So we know what their side effects are like.
"We know they work but they are given at a certain dose, and weekly, so it is not harmful. That means the patient, all being well, can be ready to start the standard treatment after six weeks."

Clinical Nurse Wendy Cunningham has been a cancer research nurse for 20 years
While not all women are suitable for the trial, even those who are eligible sometimes refuse. as it adds another six weeks to the standard round of treatment.
According to Tara, who was 31 when diagnosed and is now two years in remission, the prospect of losing her hair, while daunting, was worth it.
"I knew my hair would grow back and it has. I said 'yes' to the trial very easily.
"I was asked, 'Do you want more drugs? If it gives you more of a chance to survive, it was just an extra six weeks'. So far it's been worth it."
One of the problems around the condition is women are being diagnosed too late.
Tara said she regrets not taking up the offer of a smear test in her local GP surgery and is appealing for other women to go.
Stark warning
Richard Wilson is a consultant oncologist and a professor at the centre of cell research at Queen's University Belfast (QUB).
Prof Wilson said this it was a very exciting time for Belfast and its research into cancer.
He said there was one current area of research that is particularly exciting.
"This is a trial in ovarian cancer and it's a trial of a drug that's being developed from research in QUB.

Richard Wilson is a consultant oncologist and a professor at the centre of cell research at Queens University Belfast (QUB)
"We're giving this drug here and in two English centres to patients for the first time ever - it's a drug called ALM201.
"It cuts down the blood supply to ovarian cancer. We've finished the first phase of it and are going into the second phase."
He said the number of cancer cases in Northern Ireland is increasing as people are living longer and diagnosing cancer is improving. But he had this stark warning.
"Cancer is increasing inexorably year on year. It occurs in all ages but it is more a disease of older people. We're all living longer but are living longer to get cancer.
"Lifestyle choices are driving more cancers as well - the increase in obesity for example is fuelling cancer, so we're getting better at treating it but we're playing catch-up all the time.
Meanwhile, Tara is looking ahead.
Recently married she and her husband are planning to do a lot of travelling - she is also intending to grow her hair long again.
The trial is still recruiting new candidates.
- Published21 January 2013