Why is death rate rising for white, middle-aged Americans?
- Published

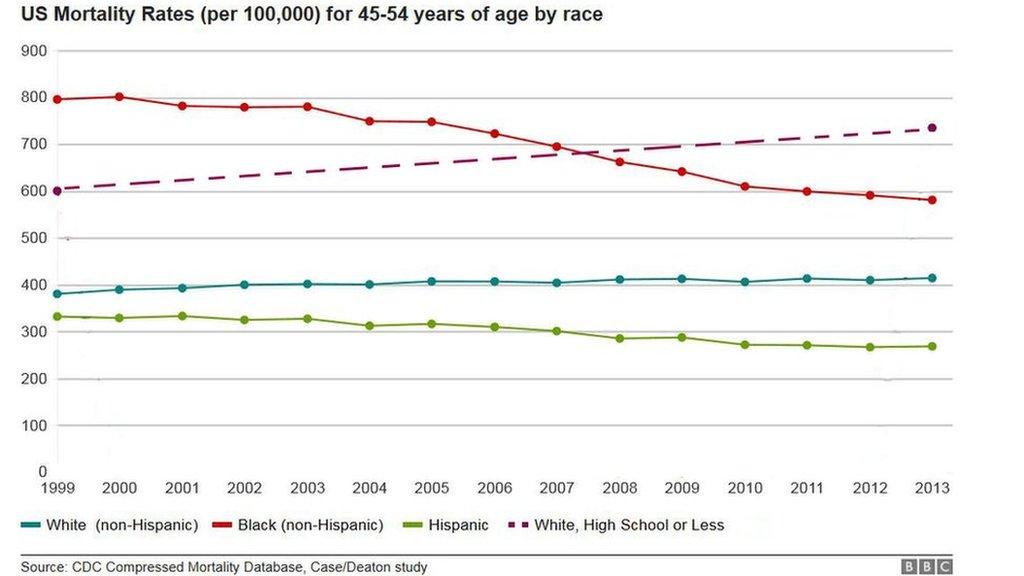
Rates of death for middle-aged white American are increasing while it decreases for other demographics
Middle-aged white Americans are seeing rising death rates that have shocked researchers. Why is this happening?
While non-whites, younger people and people in other countries are seeing falling death rates, a new study shows the reverse is happening for white men and women in the US aged 45-54.
Covering the period from 1999 to 2013, the study by Princeton University researchers says it is particularly acute for those without a college education.
"This change reversed decades of progress in mortality and was unique to the United States; no other rich country saw a similar turnaround," the authors wrote, external of their study, published in the Proceedings of the National Academy of Sciences.
So what's believed to be behind it?

Suicide

Suicide rates are higher in the Western and Southern regions of the US
National data sets from the US Centers for Disease Control and Prevention used in the study show that middle-aged whites are committing suicide at an unrivalled rate.
Suicide rates were reported to be higher in the Southern and Western regions of the US than in the Midwest or the Northeast, where people around them tend to be more highly educated and employed.
"[Increased mortality rates] really do show a growth disparity in health that reflects a growing disparity in wealth," Joshua Sharfstein, a professor of public health at Johns Hopkins University, told the BBC. "It's more than a collection of anecdotes."
But why are whites so much more likely to commit suicide than other demographic groups? Researchers say the answer is complicated - and has a lot to do with culture.
"It is striking that suicide rates are highest in white females and white males. That is a complicated social and cultural phenomenon," Pat Remington, a professor of population health sciences at the University of Wisconsin, told the BBC. "It has to do with a mix of risk factors."
Mr Remington also pointed to the widespread availability of guns and prescription drugs that enable suicide.
"This is not an urban, African-American issue as much as it is a poor, rural, white male issue... Culture comes to play, a culture of not necessarily treating depression," said Mr Remington. "The rural culture - if it's not broken, don't fix it."

Drug and alcohol abuse
A heroin addict tells how he lost his business and family
Prescriptions for opioid drugs for pain control in the US have increased greatly since the 1990s.
When opioids became harder to obtain through regulations, some people turned to heroin as the US saw rising quality and falling prices for the illicit drug.
"There are no single reasons for this, but the typical cascade is - an individual will obtain a narcotic through a prescription, transition to lower cost drugs like heroin, then eventually have health problems, then have an early death," said Mr Remington.
The New York Times reports, external that 90% of people who tried heroin in the last decade were white.
According to the newspaper's report, drug addiction in black communities ultimately resulted in mass incarceration, while heroin and prescription drug abuse has been met with calls for a more sympathetic approach, possibly because its victims are largely white.
The increase in alcohol abuse can be connected to an "underlying epidemic of pain," too, the researchers write.
"The US is suffering a major epidemic of opioids and use disorders," said Mr Sharfstein. "It has obviously gotten to the point where it's affecting overall population health statistics."
"People realise that it's affecting many, many families and all of that adds up. It's the reason why this is such a serious crisis."

Declining mental and physical health
In the study, researchers found increased numbers of declining self-reported health, mental health and ability to work.
Middle-aged whites reported problems with walking a quarter of a mile, climbing 10 steps, standing or sitting for two hours, shopping and socialising - some of which are risk factors for suicide.
People may be working blue-collar jobs which keep them inactive, working odd hours or doing hard physical labour which is taking a toll.
Mr Remington said that for much of the study's time period, people were uninsured.
"Forty-five to 54 is an age range where people can struggle. They may be in mid-life, they may not have the means, or health insurance or access to primary care," said Mr Remington.
The pattern of mortality decline slowdown is troublingly similar to what happened in the US during the height of the Aids epidemic, the researchers point out.

Financial stress
Financial insecurity weighs heavily on US workers, the researchers point out.
This particular group, without university degrees, is struggling with economic insecurity and lack of sufficient retirement funds, contributing to anxiety and overall loss of well-being.
Growth in earnings has been slow, the researchers note, and unlike Europe, where defined-benefit pensions are common, US pension plans carry stock market risk. Many have not contributed enough to their retirement plans.
As the researchers point out, economic productivity slowdown happens in many European countries, but they are not seeing the same drastically increasing mortality rates.
"With the culture in rural communities, when economic conditions [worsen] during recessions, we see almost like clockwork, rates of suicide and self-destructive behaviours going up," said Mr Remington.

- Published8 July 2015
