Vulvodynia: When a chronic pain in your lady bits controls your life
- Published
Think of your vulva - the external part of the female genitals - for a second.
Now, imagine having someone twist your sunburnt arm, and feeling that pain - down there.
That pain means you can't have penetrative sex, you struggle to sit down for any length of time and you can't wear skinny jeans or use tampons.
That's the experience of women who have vulvodynia, a condition that can be hard for some doctors to diagnose because it has no visible symptoms.
WARNING: This article contains references to sex and detailed descriptions of the female genitals
"If you imagine your perineum, so that's the space between your vagina and your anus, the bit of skin that sits just above the perineum, just at the bottom to the entrance of the vagina, is where most women get the pain," says 23-year-old Claudia, who has the condition.
"It can range from a tiny little bit [of pain] on the side, to the whole area."
Claudia first started getting the symptoms of vulvodynia when she was in her late teens but it took time for her to get the courage to go to the doctors and even longer to get a diagnosis.
For her, the pain can feel like "having a cut and having chilli rubbed into it".
The Vulval Pain Society has links to help and information about vulvodynia., external
Claudia has been with her boyfriend for a couple of years and says that having vulvodynia has had a real effect on their sex life.
"You can be as relaxed as you want, you can be totally comfortable with your partner, you really want things to happen and it just can't," she explains.
"I remember one instance where, I tried. I really wanted to have sex.
"And that was such a bad decision and I ended up sitting in a cold bath for two hours trying to get the burning to stop."
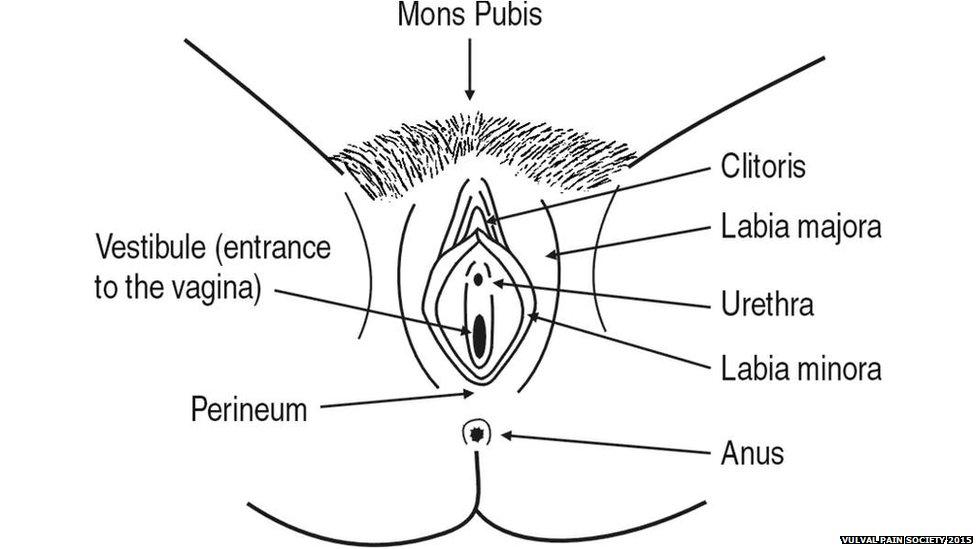
The vulva is the entire area of the female genitals
Although Claudia says the impact on her sex life is huge, that's not the only way vulvodynia affects her.
When her symptoms are bad she can't cycle, wear any tight-fitting clothes, or even sit down for a long time on public transport.
"I couldn't wear skinny jeans and then walk to the bus stop, it would be seriously uncomfortable," she says.
While it took her some time to find a doctor who understood her condition, she is now on a treatment regime that has had some success.
"When I was first diagnosed, I'd go and see a physiotherapist who effectively gave me NHS-sponsored dildos of different sizes and said use these on your own, at your own pace and just get your body used to the idea that just because it's going in doesn't mean it has to hurt," she says.
She is also on strong painkillers, which means she can't drink alcohol.
"There was definitely a period where I felt, well, 'I can't have sex therefore I'm not actually a woman.' I'm not living up to what is expected of me and that made me feel awful.
"I tend to wear the most boring cotton knickers because I know that if I deviate things are likely to go wrong.
"My boyfriend was like, 'Why don't you get some nice underwear?' It feels like false advertising because I know that whatever I wear, whatever I look like, I can't actually fulfil that.
"It felt like I was leading him on."
There are no official statistics on how many women in the UK are affected by vulvodynia.
The NHS says it usually affects women of all ages, external, from 20 to 60 and symptoms often start before the age of 25.
Vulvodynia is different from, but can cause, vaginuismus. This is when the muscles tighten around the vagina whenever penetration is attempted.
A study of almost 5,000 people, carried out in the US, suggests that about one in six women, external have experienced the symptoms for more than three months during their lives.
Fewer than half of the women in this study got an official diagnosis and many did not seek any medical help at all.
Part of the problem when it comes to diagnosis is that vulvodynia does not typically have any visible symptoms.
"They may have gone and seen, usually a GP, and an examination doesn't reveal anything to see," says Ms Deborah Boyle, a gynaecologist who has expertise in treating vulval pain.
Part of Ms Boyle's work involves educating other doctors about vulval pain and she says that many of them are "not absolutely sure what goes where" when she asks them to do an anatomical sketch of the vulva, making understanding the condition even more difficult.
BBC Advice has more information about the vulva and vagina.
There are a number of theories as to the causes of the condition including injury to the nerves, allergies or being very sensitive to yeast infections (thrush).
Ms Boyle says one explanation that is often given is that sufferers have a history of sexual abuse.
"In my clinical experience that is not the case. It is sometimes, but it is by no means the majority of the women who are suffering," she explains.
Follow @BBCNewsbeat, external on Twitter, BBCNewsbeat, external on Instagram, Radio1Newsbeat, external on YouTube and you can now follow BBC_Newsbeat on Snapchat