Strain and impatience - life inside a GP practice

Jackie Springett says patients' attitudes have changed during her 21 years as a receptionist
- Published
Anne-Marie Tasker spent a busy Monday morning with the staff at a rural GP practice to see for herself what demand for its services is like.
Staff at a North Lincolnshire GP practice say they are "busier than ever” and saw more than half their registered patients last month.
They say summer has not brought a drop in demand at the Kirton Lindsey & Scotter surgeries, with the added pressure of patients on hospital waiting lists needing pain management.
"I used to have an hour for lunch. Now I eat at my keyboard and work all day. I don't leave the room, except maybe to go for coffee," says senior GP partner Dr Satpal Shekhawat.
Jackie Springett, practice receptionist for 21 years, says patients are more demanding than they used to be. She adds: "People don't want to wait for anything."
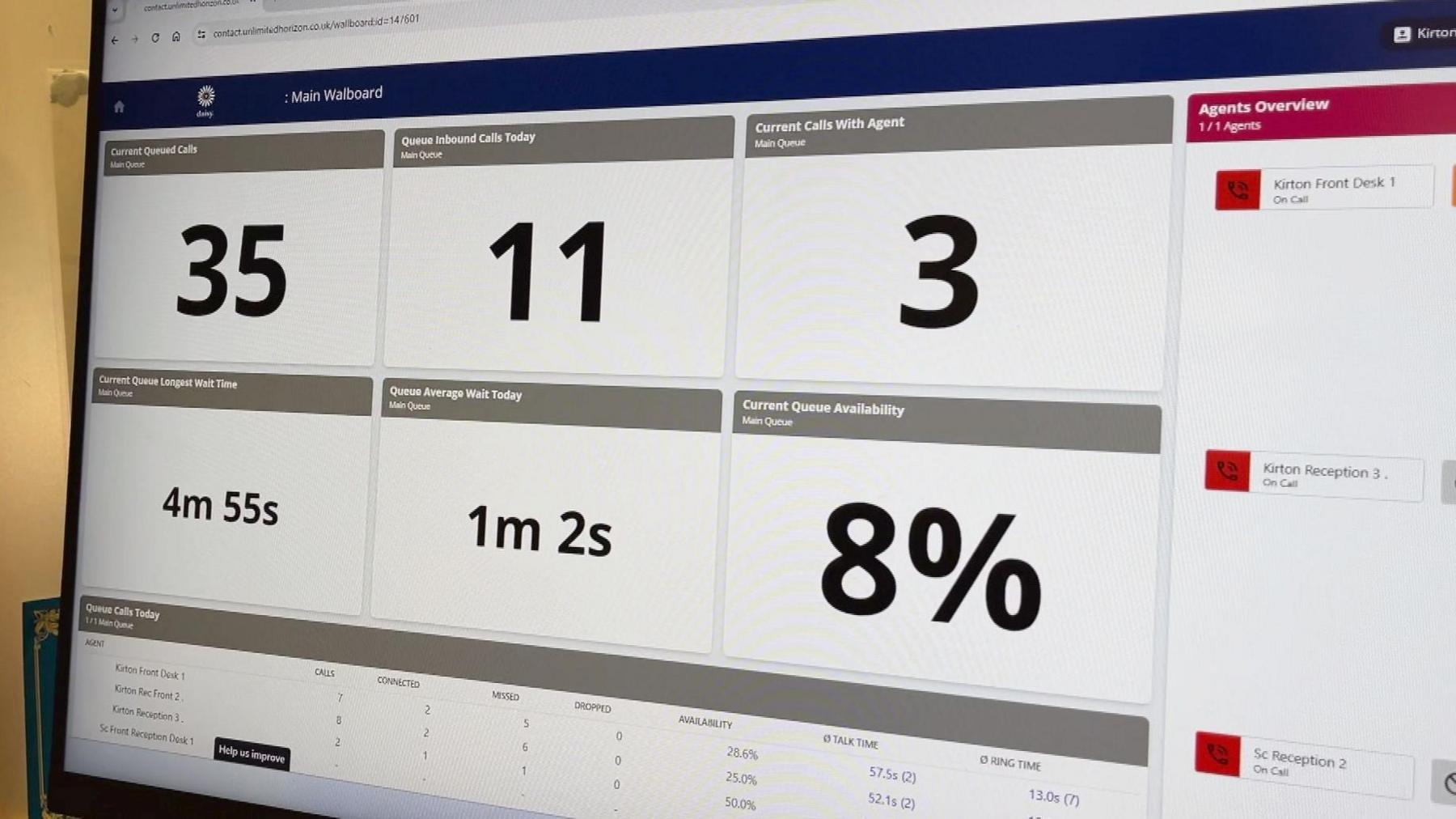
By 8.10am, 35 patients are queueing on the phone lines
Ms Springett dreads Monday mornings and finds it stressful knowing there could be queues of callers both on the phone and at the door.
"It does affect me knowing I have to come in to that first thing on a Monday and that I may not be able to offer everything that people want or expect," she says.
"That gets me down."
She is one of six staff answering the calls across the two surgery sites, and sits in the shadow of a large screen displaying the number of calls waiting.
Ten minutes after the lines have opened, 35 people are in the queue. Within an hour, 85 calls have been answered.

Nurses and other healthcare professionals carry out 53% of the practice's appointments
Ms Springett says it has got busier, and patients are reluctant to see anyone but a GP.
"You point people in the right direction to get help elsewhere besides coming here. They don't always like that. They want to see a doctor," she says.
"When you say we have a pharmacy consultation, they don't really like it."
She adds that some patients try to book on-the-day emergency appointments, regardless of need, "because they have no patience and they don't want to wait".
"When the appointments run out and I have to tell people we haven't got any left, or they have to use the online triage or go to the pharmacy, they don't like that and I take it to heart," she adds.
"I know it shouldn't, but it does affect me. It's hard on me, it's hard on any of the staff members. It is a lot more difficult than it used to be."
In May, 51% of the practice's registered patients had an appointment - some to meet the growing demands from hospitals to carry out tests and prescribe on their behalf.
Dr Shekhawat says that although the number of appointments the practice offers has increased by more than 20%, the budget has not, and that helps determine whether a patient can see a doctor or needs to be treated by another health professional.
"To employ GPs, it costs us more. Our financial budgets have not been increased in line with the increase in cost," he says.

Dr Satpal Shekhawat says he has time to leave his room only to get coffee
He explains that although the waiting room might have only a few people in it at any time, the practice is "busier than ever".
"The waiting room can be empty due to staggered working hours. We're doing longer days, we start late, finish late, different practitioners are working at different times," he says.
"We get a lot more online questions. We have blood results to file. We have hospital letters to look at. We have to order or arrange medications which specialists have recommended.
"All that work is still ongoing inside the doctor's room, without the patient being in the building, so it may look empty - but I can tell you, we have no time!"

Patient Louise Swindles says three-week waits for appointments are 'annoying'
The majority of the patients going through the waiting room have same-day appointments with a nurse or a GP.
One of them is Louise Swindles, who has filled a cancellation slot, but she says the wait for a routine appointment can be weeks.
"It's frustrating. I booked an appointment for my son and that was three weeks' wait," she says.
"It's not an emergency, but he wants to be seen and it's annoying, but we have to put up with it. The NHS overall is struggling."
Another patient, Beverley Altoft, says getting an appointment with the nurse was "dead easy" and she was seen just two hours after calling the surgery.
She says that "sometimes you can be 30th in the queue", but "nine times out of 10" she manages to get a same-day appointment.
She adds that she is happy to see healthcare professionals other than a doctor.
"I did say I would see the pharmacist, but they listened to what I said and the receptionist said, 'No, I want you to see the nurse and if she isn't happy, she'll call the doctor in', so they covered me every way."

Patient Beverley Altoft says 'nine times out of 10, I'm seen the same day'
Dr Shekhawat says more patients having that attitude would be one step towards addressing the growing crisis in GP care.
"I think one thing won't solve it. It will be a collection of things and that will include financial support, better recruitment and education for patients to use the services better as well," he says.
"In our practice, the doctor triages and the patient is sent to the most appropriate person. If somebody thinks their wound is infected, they don't need a GP. My nurse can equally - or maybe better than me - check the wound and dress it.
"Similarly for colds and other illnesses, the pharmacist is appropriate.
"I want to get the message out: if any of these practitioners feels the patient needs to see the GP, they have access to call us, to send the patient back to us, so nothing is unsafe."
Ms Springett agrees.
"I think even if I had loads of appointments, I don't think it would satisfy the people that are ringing in to book," she says.
"Patients need to get used to going to other places to be seen, not just the GP."
To see what each party is proposing regarding the future of the NHS, visit the BBC manifesto page.
Related topics
- Published21 June 2024

- Published13 October 2023

- Published9 May 2023
