'Cancer trial has given me my life back'
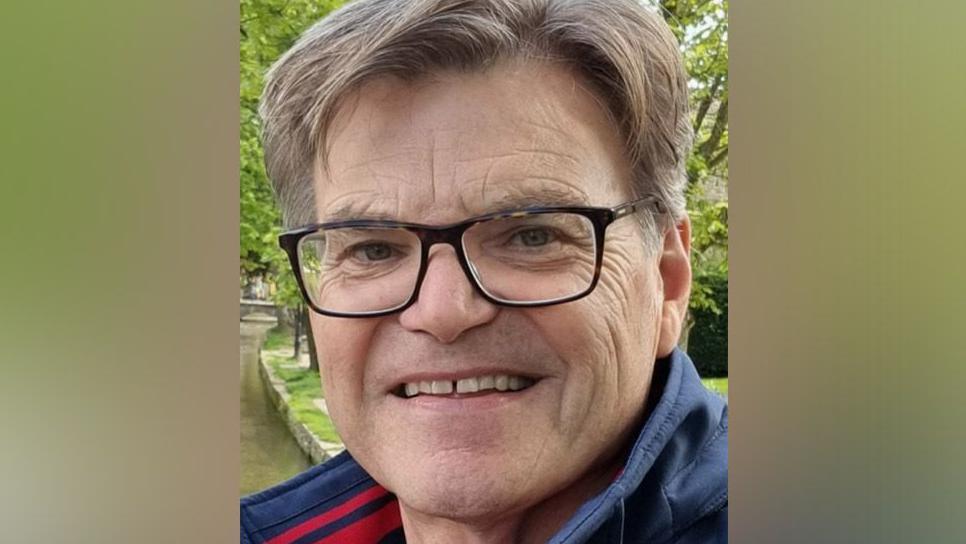
Gordon Nash says the clinical trial has improved the quality of his life
- Published
A throat cancer survivor says a pioneering clinical trial has "helped me get back to enjoying life with my wife".
Gordan Nash, from Merseyside, was diagnosed with HPV positive throat cancer in 2018 ago after finding a lump when he was shaving.
He signed up to the Pathos trial, external, offered by the Liverpool Head and Neck Centre, which looks at how these cancers can be treated to minimise the long-term side-effects for survivors.
Mr Nash is now urging others to take part in clinical research if they are eligible.
One of the main side effects for people having treatment for head and neck cancer is a deterioration in their ability to swallow, Prof Terry Jones, the director of Liverpool Head and Neck Centre who is leading the research for the Pathos trial for the University of Liverpool, explained.
Rates of these types of cancers in Liverpool are reported to be up to three times higher than the rest of the country, according to North West Cancer Research.
For Mr Nash, 62, it meant having reduced radiotherapy which he said has improved his quality of life.
Mr Nash said: "The radiotherapy is probably the hardest part.
"Most people, even myself, think the surgery's going to be the toughest part and it really wasn't.
"Your throat gets very sore. It's difficult to swallow."
He said: "It's very intensive so I 100% understand the reason for that research because if they can shorten the timeline for the radiotherapy, then there's going to be less damage and less discomfort during the treatment."
The building engineer said: “I was fortunate that, following the initial investigative surgery and scans, my consultant advised me that treatment would likely mean I would be cured of my throat cancer.
“He also said that I could take part in the Pathos research study as part of my ongoing care."
He said it was a "huge relief".
"I don’t think I have ever experienced such a release of emotion and I was able to go into the trial with a positive attitude."
He thanked the "amazing NHS team that has helped me get back to enjoying life with my wife, playing guitars and going back to the gym".
He urged others to take part in clinical research "if it is offered to you".
The trial, being offered at hospitals across Liverpool, in collaboration with the Liverpool Head and Neck Centre, is the biggest head and neck cancer research study in the world.

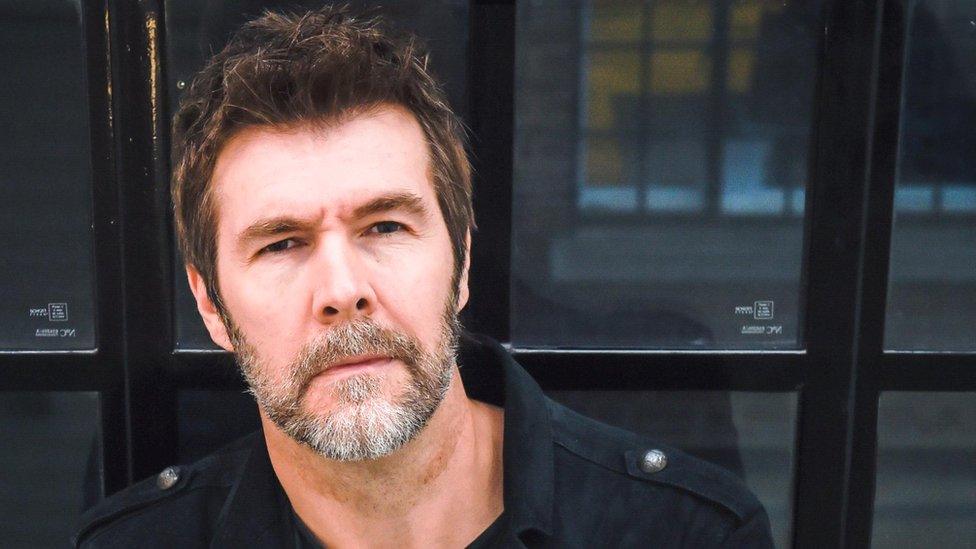
Stuart Keane ringing the bell to mark the end of his treatment
Stuart Keane, also from Merseyside, was told he had head and neck cancer two years ago.
The 59-year-old also found a lump whilst shaving and needed surgery to remove the tumours.
Mr Keane then started radiotherapy and chemotherapy for six weeks.
He has since been told he is cancer free.
His consultant at Aintree Hospital, Prof Jones, asked Mr Keane if he would take part in the study which is the world's largest head and neck cancer study.
He said taking part in the trial has "given me a lot more mental security" as he has been in hospital and "I'm constantly checked up on it".
He added: "It's reassuring, but also it's the opportunity to give something back."
Prof Jones said: "Patients who enter the trial have surgery just as they had before and then, depending on the outcome of that, they end up having either normal standard of care treatment or de-intensified treatment afterwards.
"When the trial is over we'll be able to see whether in fact our original hypothesis was true that that de-intensifying treatment will actually lead to similar survival outcomes but better swallowing function," he said.
The trial - which is funded by Stand Up To Cancer campaign for Cancer Research UK has been running since 2015 - ends in October - with more than 1,000 patients taking part.
The results will be out three years later and it is hoped it will change how these types of cancer are managed across the world – and improve the lives of patients.
Listen to the best of BBC Radio Merseyside on Sounds and follow BBC Merseyside on Facebook, external, X, external, and Instagram, external? You can also send story ideas to northwest.newsonline@bbc.co.uk, external
Related topics
- Published10 March 2024
- Published1 November 2023

- Published22 March 2024
