'Antibiotic-resistant superbug left me with the hip of a 70-year-old'
Pharmacy student Amy Symington was a fit and healthy hockey player until she became ill in February 2024
- Published
A 21-year-old student who had to learn to walk again after being struck down by an antibiotic-resistant "superbug" has said she has been left with the hip of a 70-year-old.
Amy Symington developed MRSA, external in February 2024 after an abscess in her hip became septic but the bacteria was difficult to treat due to antimicrobial resistance, external.
Known as AMR, it occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines. As infections become harder to treat, it increases the risk of disease spreading, severe illness and death.
Northern Ireland's Public Health Agency said AMR has been identified as one of the most pressing global health challenges of this century, external.
Amy, from Portstewart, County Londonderry, was a keen hockey player - fit and healthy with no underlying health conditions - until she took a dull pain in her hip.
It deteriorated to the point she "couldn't walk". She said she had "never experienced pain like it".
After flying home from university in Manchester, Amy ended up in hospital where she was diagnosed with sepsis and MRSA.
"I just remember vividly in school learning about MRSA and our teacher describing it as a superbug, which was one that's resistant to a lot of the antibiotics that they use to treat all sorts of infections," she said.
"I think that set in a whole other level of panic."
The then 19-year-old said her first night in hospital was "one of the most frightening days" as she "didn't know whether I was going to make it through the night".
She said it was "trial and error" to find the right treatment for the infection and that once that happened "everything started to come back down to normal thankfully".
Amy said getting the right combination of antibiotics was "determining whether I lived or not".
"I just think it's really important that we keep these types of medicines working because I won't be the last one that's going to rely on them," she said.

Amy said it was trial and error for doctors when seeking to find a medicine that would work to treat the infection
"It definitely it took a while for me to really feel like myself again.
"I had to learn how to walk again.
"I was with the physios every day just taking it day by day and really didn't notice a big improvement until after I left hospital.
"By this time, it had been well over a month that I really couldn't walk properly at all and to go from being someone that was doing every sport under the sun to being in that situation was definitely hard."
Amy spent four weeks in hospital and was left with a badly damaged hip joint and arthritis.
She said she will need a hip replacement as it is the "only resolution to solving the pain that I get in it".
The pain means she still walks with a bad limp.
"The doctors describe it as having a hip of a 70-year-old," which she said is "hard to believe".
"I didn't think I would be left with that much damage.
"Obviously the pain at the time was bad, but even now the aftermath, some days the pain is so unbearable and it's really quite hard to live with," she said.
Now 21, the third-year pharmacy student said while she has accepted she is not going to go back to playing hockey at the level she was, she is hopeful, with further treatment, she will have a "pain-free hip one day".

Amy has accepted she will not play hockey again at her pervious level
Antibiotic resistance 'a catastrophic threat'
Bronagh McBrien, programme manager in the PHA for antimicrobial resistance, warned that, like Amy, anyone can pick up an infection that becomes much more severe if antibiotics cannot treat it.
She said the introduction of antibiotics was "one of the greatest medical breakthroughs" in history but that AMR is a "catastrophic threat" that requires us to "use our antibiotics responsibly to make sure we can save them for future use".
According to the World Health Organisation (WHO), external, it is estimated that bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths.
Ms McBrien said AMR makes standard procedures and treatments - like caesarean sections, hip replacements and chemotherapy - much riskier.
"It is quite a big burden on society and without antibiotics, we're going back to the days where we didn't have anything to treat [infections] and carry out normal medical procedures," she said.
"Ultimately we don't do the risky procedures or when we do them and people pick up infections, they will die from infections."
Ms McBrien said it is a "real challenge" as there is not a "pipeline of new antibiotics" coming on the market that can treat resistant infections.
"That's why when people are picking up these resistant infections we're running out of options," she said.

She added that everyone has a part to play in limiting AMR by using antibiotics responsibly.
This means not using them for minor ailments and common infections but using over-the-counter medicines instead; taking antibiotics according to your doctor's instructions; and not taking antibiotics that have not been prescribed to you.
Antibiotics are no longer routinely used to treat infections, external.
A new UK AMR National Action Plan 2024-2029, external includes ambitions to reduce total antibiotic use in human populations by 5% from the 2019 baseline and investments in new tools and technologies to develop long-term solutions.
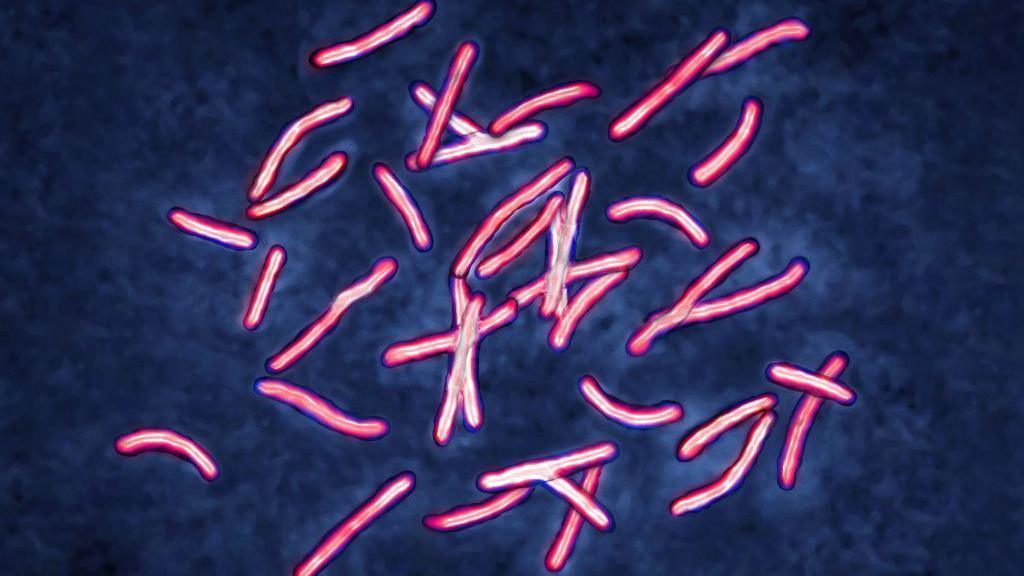
What are 'superbugs'?
The overuse of antibiotics, external in recent years means they are becoming less effective and has led to the emergence of "superbugs".
These are strains of bacteria that have developed resistance to many different types of antibiotics, including:
MRSA (methicillin-resistant Staphylococcus aureus)
Clostridium difficile (C. diff)
the bacteria that cause multi-drug-resistant tuberculosis
These types of infections can be serious, challenging to treat and are becoming an increasing cause of disability and death across the world.
- Published20 February
- Published22 November 2022

- Published12 April 2022


