Nurses bore the brunt of Covid, ex-chief nurse says
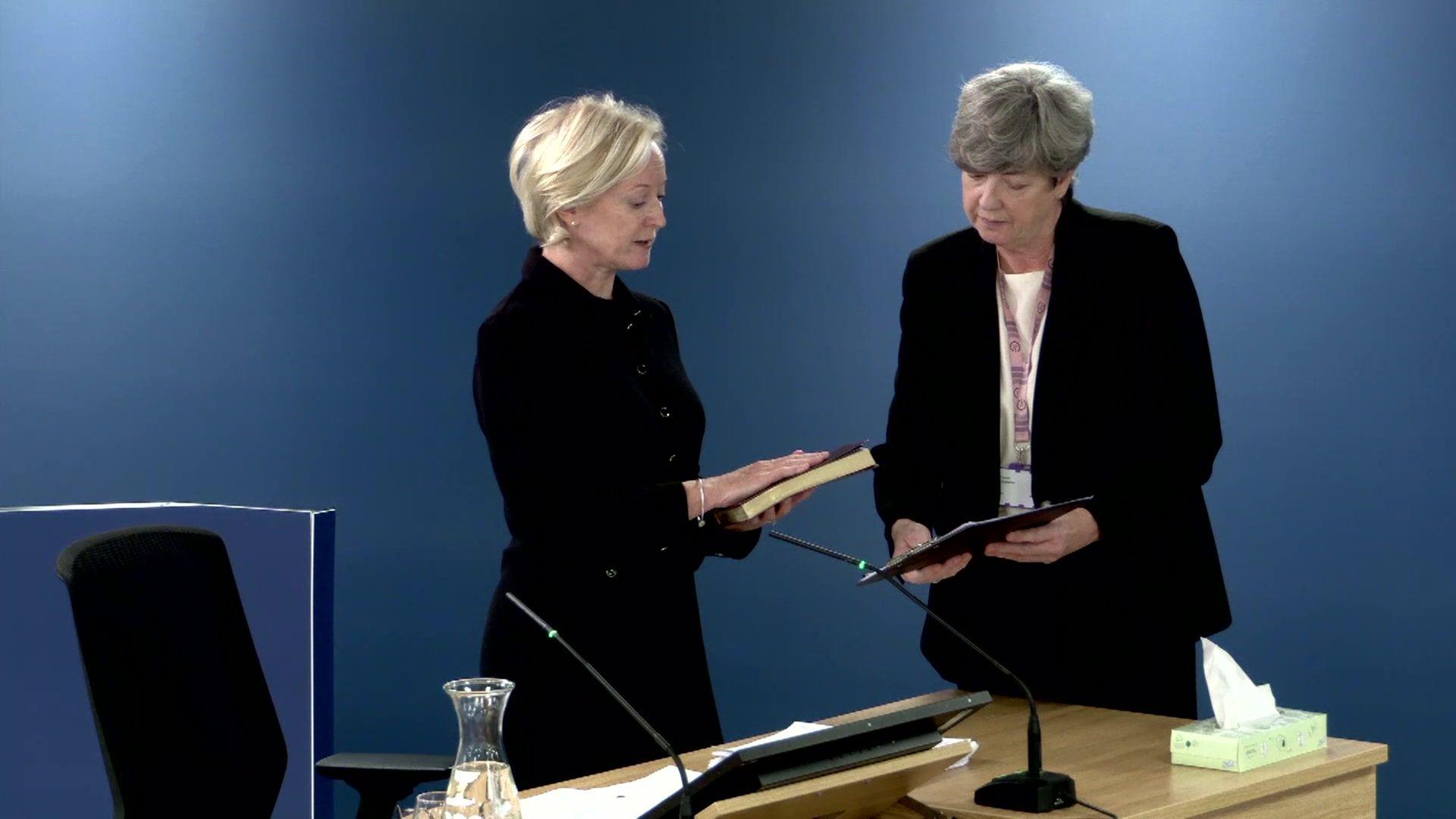
Dame Ruth May was England's chief nurse from 2019 until she retired in July 2024
- Published
Nurses bore the brunt of the pandemic, with low staffing levels and difficulties accessing protective equipment, according to England’s former chief nurse.
Dame Ruth May told the Covid inquiry the NHS had been understaffed in 2020, in part because of the “catastrophic decision” to cut financial support for student nurses in 2015.
Resources had been "stretched", particularly in intensive care, she said, with a knock-on effect on the care some Covid patients received.
And she had been aware of widespread reports of problems supplying personal protective equipment (PPE) in March 2020, including a shortage of plastic gowns that had left front-line nurses living "in fear".
‘Fast-moving environment’
Dame Ruth, England’s chief nurse from 2019 until July 2024, was one of the senior figures who appeared at Downing Street news conferences during the pandemic.
She had also volunteered for nursing shifts during Covid, at times working "under the radar" in hospital wards, the inquiry heard.
“We were facing some extraordinarily difficult decisions in the very early part of pandemic,” she said.
“It was a fast-moving environment - we were seeing [a large] number of cases coming in and deaths like we had never seen before.”

Dame Ruth May alongside former Health Secretary Matt Hancock and former Health Minister Nadine Dorries in April 2020.
The NHS had entered the pandemic with about 40,000 nursing and midwifery vacancies in England, Dame Ruth said.
And she criticised a “catastrophic decision”, in 2015, to replace the grant or bursary paid to student midwives and nurses with loans.
It had led to reduction of about 5,700 trainees in England by 2020, Dame Ruth said, which “would have made a difference” in the pandemic.
“There would have been less burnout - there would have been less psychological impact,” she said.
Intensive-care units came under such pressure during Covid specialist critical-care nurses were responsible for up to six patients each instead of the usual one-to-one ratio.
And Dame Ruth accepted that had affected the care patients received, saying: “It was not where we wanted to go... and I know there have been consequences because of it.”
Blanket do-not-resuscitate orders had appeared to have been added to some patients’ records based on either their age or a pre-existing condition such as autism or a learning disability, she told the inquiry, which had been “completely wrong”.
Online abuse
Dame Ruth also suggested it had been a mistake for some hospitals to prevent pregnant women from being accompanied by their partners during scans or the early part of labour.
The faster rollout of Covid tests would have allowed visitors to come back into hospital earlier and been safer for staff and patients, she said.
Dame Ruth also spoke about the “pretty horrible” online abuse she had faced at the time.
“The one thing I learned about the whole of this [period], is the importance of integrity - and sometimes that comes at a cost,” she said.
“That means on social media in particular you are vilified - [but] I wasn’t the only one.”
The Covid inquiry is currently taking evidence about the impact on the NHS and healthcare systems across all four nations of the UK.
More than 50 witnesses are expected to appear in this third section or "module", which runs until the end of November.