Hospices' plea for funding as services are slashed

Hospices like the Lewis-Manning Hospice in Poole specialise in palliative care but also provide other services
- Published
Hospices say the sector urgently needs better funding, whether or not the assisted dying bill becomes law.
Hospice UK which represents more than 200 sites warns that 40% its members will have to make cuts next year because of surging costs.
CEO Toby Porter says hospices are stopping certain services just as demand is rising, with an ageing population.
The Government says it is investing more than £100m to improve hospice facilities.

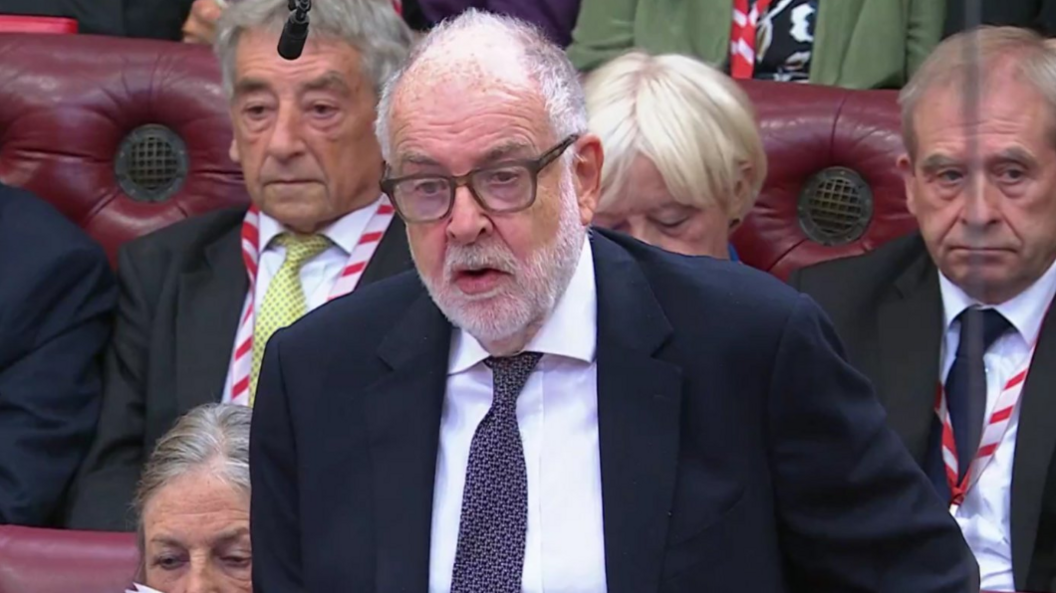
Toby Porter, CEO of Hospice UK, says the industry is still unclear about its role if the assisted dying bill becomes law
Mr Porter says there are a number of unanswered questions the sector has over its role, as the bill passed its second reading in the House of Lords.
Those questions include what level of involvement hospices will have and if it will be compulsory to provide assisted dying or they can opt out.
"Over the last three years, hospice charities have seen accumulated cost pressures, but the money that they've received from the government has stayed flat, and that's seen services cut back," Mr Porter said.
"What would it say about us as a country if someone decided to opt for an assisted death because they were worried that they wouldn't be able to get the care they needed to control their pain or manage their symptoms, or that their family wouldn't be properly supported?"

Clare Gallie is CEO of Lewis-Manning Hospice says relying on public donations is not sustainable
'Everyone is affected by end-of-life care'
Lewis-Manning Hospice in Poole says it is feeling the pinch like many others in the charitable sector.
CEO Clare Gallie revealed the hospice relies on contributions from the public as government funding only covers 12% of its costs.
"The one certainty in life is that we're going to die, so why not invest in that and make that the best death that can happen for anybody in our community," said Ms Gallie.
"Palliative and end-of-life care is something that's going to affect absolutely everybody and what's really important is that there's the funding and the sustainability to match that."

Laura Adams is Director of Nursing at Lewis-Manning and says care is based on listening carefully to patients' requests
Laura Adams is Director of Nursing at Lewis-Manning and said staff are unable to support as many people as they would like.
"We focus on living," she said. "We work hard to demystify what a hospice is - it isn't about dying - we see people here who are well enough to attend our clinics.
"If there is a state-funded assisted dying service, really as a hospice and a palliative care team, we should be one of their safeguards."

Lisa Salamon is a patient at Lewis-Manning Hospice and is worried about services being cut
Lisa Salamon was first diagnosed with breast cancer ten years ago.
She is in remission and is not dying, but still visits the hospice regularly as she needs daily treatment for Lymphedema, an incurable condition caused by her cancer treatment.
"You have good days and you have bad days - some days I do get up and my big toe hurts and they're (hospice staff) always there for me.
"When you finish your oncology in Bournemouth Hospital, they send you to Lewis-Manning.
"If these are completely cut, where are we supposed to go?" Ms Salamon asked.
Get in touch
Do you have a story BBC Dorset should cover?
You can follow BBC Dorset on Facebook, external, X (Twitter), external, or Instagram, external.
Related topics
- Published19 September
- Published14 May
