Nature and outdoors increasingly prescribed by GPs

Dr Divya Kuttappan says she regularly uses social prescribing for benefits that "can't be addressed by medicine alone"
- Published
There has been a rise in doctors prescribing nature, outdoors and community activities to tackle mental illness in Lincolnshire, NHS figures show.
Social prescribing connects patients with community groups that run outdoor activities and other voluntary programmes.
Prof Rob Poole, who established The Centre for Mental Health and Society, has criticised the idea as having "little evidence" to support its use.
However, Dr Divya Kuttappan, of Parkside Medical Practice in Boston, Lincolnshire, regularly uses the method and said "engaging in activities and being part of a community creates a new sense of purpose, which can't be addressed by medicine alone".
Social prescribing is described as a "key component" of NHS England's plan, external.
It hoped to refer 900,000 people in 2023-24.
In Lincolnshire, its use has increased from 128 people being referred as part of a pilot in 2017-18 to 4,584 in the 12 months leading to March 2024, according to NHS Lincolnshire Integrated Care Board.
Dr Kuttappan added: "There is no one condition that we refer to social prescribing.
"We just get an idea by speaking to the patient that they would benefit from certain things other than the prescription that they normally have.
"I don't think it is to avoid prescribing medication, it is to go alongside it.
"In some cases we can avoid prescribing medication just by encouraging them to engage in these activities."
Some studies, external have said the idea has led to "improvement in mental wellbeing" for patients.
But Prof Poole, who teaches social psychiatry at Bangor University, co-wrote a paper suggesting there is "little evidence for its effectiveness", external.
He said: "It's a very large investment and we would want to see a large public health gain. There is no grounds to believe that there will be a large public health gain."
Prof Poole also criticised the policy for largely benefitting the middle class, but said it is not going to "help the people who most need help".

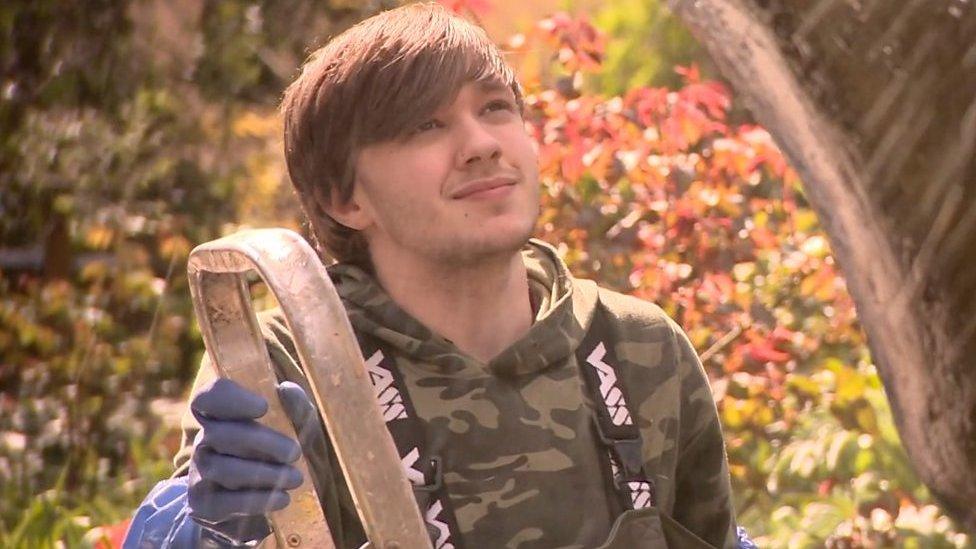
Peter Gregory was referred to a community allotment for help with his mental health
Peter Gregory, who had been struggling with his mental health after the death of his father last year, is one patient who has seen the benefits first-hand after admitting "everything just seemed to fall apart".
"I didn't want to go out, or see or speak to anybody," he said.
"Through the doctors I spoke to a nice lady who helped me get in contact with Willoughby Road Allotments. They helped and supported me through this.

Willoughby Road Allotments, near Pilgrim Hospital, helps people via Social Prescribing
"Now, it's made me decide to try and start my own gardening business.
"You might not want to try it, but just try it, try persevering with it and carrying on. It's definitely worth it. It has helped me such a lot."
Listen to highlights from Lincolnshire on BBC Sounds, watch the latest episode of Look North or tell us about a story you think we should be covering here, external.
Related topics
- Published25 November 2024

- Published1 August 2024

- Published18 April 2023
- Published28 October 2024
