'NHS cut funding after Gran didn't die on time'

Pearl has advanced dementia and had been receiving NHS Continuing Healthcare for two years
- Published
A woman has accused the NHS of withdrawing funding for her 98-year-old grandmother's care because "she didn't die on time".
Pearl, from Bradford, has advanced dementia and was fast-tracked onto NHS Continuing Healthcare (CHC) in 2023 to support her at home after a hospital admission.
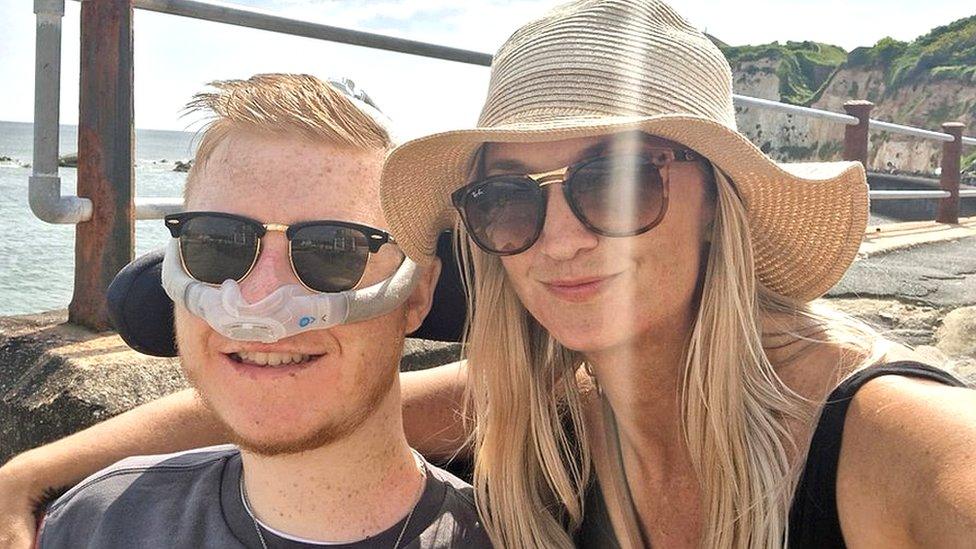
Her granddaughter, Kirstie Lumley, said she was now being left to "die without dignity" after funding was stopped when a review found her needs were no longer primarily health-related.
The West Yorkshire Integrated Care Board (WYICB) acknowledged its funding decisions could cause "disappointment and distress" but added they were "based on an individual's assessed needs, not their diagnosis or financial situation".
In June 2023, Pearl's family were told she required end-of-life care after being discharged from hospital following a urinary tract infection.
At the time she was deemed eligible for fast track CHC, which allows quick access to NHS funding for patients who have a "rapidly deteriorating condition" and "may be entering a terminal phase".
Last month, following a review of her case, the family was told that funding would cease on 1 August 2025.
Ms Lumley, from Malton, North Yorkshire, said the decision felt "unfair" because her grandmother's condition was "certainly no better" than when she was originally funded.
"She was expected to pass away in 2023 when she was discharged from hospital with an estimated prognosis of six weeks," she said.
"Because she's outlived that by a huge period of time, it's like she hasn't ticked the box and died on time."

Pearl was living independently until five years ago but is now completely bedbound
Pearl had been receiving 86 hours of NHS-funded care each week, which her family had been topping up with an extra 14 hours of care paid for privately.
Bradford Council, which has now taken over responsibility, has said she will receive just over 19 hours a week, which the family will have to pay towards, meaning they can no longer afford extra private care.
It also means Pearl will no longer have a carer to sit with her overnight and will instead have one 30-minute visit for toilet needs.
Since the changes, she has already fallen out of bed once in the middle of the night, requiring paramedics to be called.
"She's scared, she's upset, she's confused," Ms Lumley said.
"Knowing that she might be in that state and be upset and shouting out for help for another five or six hours until a carer arrives, who will only be with her for half an hour, it's just heartbreaking," she said.

Pearl fell out of bed less than a week after changes were made to her overnight care
NHS data, external shows that at the end of March 2025 more than 51,000 patients in England were eligible for CHC, with almost a third qualifying via the fast track route.
National guidance, external states there may be situations where it is "appropriate to review eligibility" for fast track CHC but goes on to say that where a patient is "expected to die in the very near future" the ICB should continue to take responsibility for the care package.
Dementia UK has launched a Fix the Funding, external campaign, which is calling on the government to urgently review the assessment process for CHC, which it believes is flawed and does not recognise the needs of people with dementia.
Andy Pike, deputy director of campaigns, said: "For people living with dementia CHC can be an absolute lifeline, but some people will end up living in situations where they may spend the last few years of caring for somebody trying to fight the system.
"We've had it described to us as 'wading through treacle' in order to try and get the outcome you want, rather than spending that time with the person you love."
The Department of Health and Social Care said responsibility for decisions about CHC funding lay with Local Integrated Care Boards, but as part of its 10 Year Health Plan it would be moving more healthcare out of hospitals and into the community, to ensure patients could access the care they needed.
'Disappointment and distress'
Meanwhile, a spokesperson for WYICB said: "We have a responsibility to ensure that continuing healthcare decisions are fair, transparent and based on assessed need in accordance with the National Framework for NHS Continuing Healthcare and NHS-funded Nursing Care.
"Decisions are based on NHS continuing healthcare assessments that are carried out by trained professionals using a nationally defined process.
"Decisions are based on an individual's assessed needs, not their diagnosis or financial situation.
"These assessments often involve people who are frail or have multiple needs, with families and carers providing considerable support.
"We appreciate that continuing healthcare decisions can be significant for individuals and families, especially in complex and sensitive circumstances, with outcomes potentially causing some disappointment and distress.
"While we cannot comment on individual cases, we can confirm that we are reviewing the matters raised here in line with our policy and complaints process."
- Published14 February 2024

- Published7 August 2023