Implant statistics warning
- Published
- comments
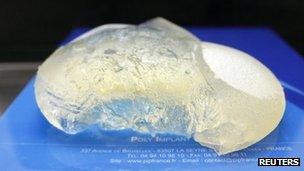
PIP implants were banned in 2010 as they contain unauthorised silicone filler
I would urge caution over some of the figures for rupture rates of the banned PIP breast implants.
In the past few days there have been claims, external suggesting that around 7% of the implants have ruptured.
But that is misleading as it is based on one small group of patients.
The Transform cosmetic surgery group has issued a statement saying the rupture rate relates to seven out of 108 patients it fitted with PIP implants since 2005.
The statement says: "This is therefore far too small a sample to provide a robust statistical analysis."
Rupture rate
It appears to be these figures which prompted the health secretary Andrew Lansley to set-up an expert committee to review the safety data on PIP implants. The committee, which meets on Wednesday, will be attempting to determine what the overall rupture rate is among the 40,000 or so women fitted with PIP implants.
The trade body which represents private hospitals and clinics described the 7% rupture rate reported in recent days as misleading. Sally Taber, Director of The Independent Healthcare Advisory Services, (IHAS) said:
"Following an audit of our members, which includes data on thousands of patients from leading groups including Transform, The Harley Medical Group, Spire Healthcare, BMI Hospitals and The Hospital Group, we can confirm that the average rupture rates reported for PIP implants is within the industry standard of 1-2 per cent."
Last week the medical watchdog the MHRA was quoting a figure of around 1% as an average rupture rate for PIP and other implants.
This was one reason why the MHRA and health ministers decided not to follow the French lead and recommend the removal of the PIP implants.
In France, the reported rupture rate is 5%, although I have also seen reports that the rate there is 3.6%.
Tim Goodacre, president of the British Association of Plastic, Reconstructive and Aesthetic Surgeons and an Oxford University lecturer said even a rupture rate of 1% would be high:
"If you have an implant the likelihood that you will need follow-up surgery is about 1% per year. But that can be for a whole range of reasons. Ruptures of implants are, in my experience, rare. After 10 years 10% of women will have needed follow-up treatment, but 90% will not."
Mr Goodacre is one of a number of surgeons on the expert panel meeting tomorrow.
Implant register
Several groups are calling for a registry of implants. Sally Taber from IHAS suggested this should work along the lines of the National Joint Registry, external.
This was set up in 2002 and records the details and outcomes of all hip, knee and ankle replacement surgery in the NHS and private sector.
A breast implant registry did operate from 1993-2006 but was eventually shut because only a small proportion of women were willing to take part in the scheme.
Sally Taber said every patient must be prepared to have their data recorded, which would need to be anonymised.
We may never know exactly how many women in the UK have PIP implants. Although clinics and surgeons are required to record information, many firms have gone out of business.
A national register of implants would allow women to get information from a central database, bypassing the firm which treated them.
Tim Goodacre agrees that a registry would improve standards: "At present we can't easily say how many PIP implants were done, where and how well. We must have traceability so that even if a company goes bust, the device can be traced."
Another surgeon on the PIP expert committee said there are no firm figures on what proportion of PIP devices have ruptured.
Fazel Fatah, president of the British Association of Aesthetic Plastic Surgeons said: "None of these figures are completely reliable or are a true reflection of what's happening. A significant number of patients do not go back to the clinic where they had their surgery if they suffer a rupture. Instead, they go to the NHS and are dealt with in the NHS. We do not know the exact rupture rate in the UK."
Mr Fatah said he believed women should plan for having implants removed. "The point is not so much the rupture rates but that the quality of the silicone in these implants is not of medical grade. Therefore, the implants are not fit to be implanted into humans."
'Moral obligation'
He said women should not be caught in the middle of an argument over who should pay for the implants to be removed, adding that clinics who carried out the surgery had a "moral obligation" to women and must not be allowed to profit from removing the devices.
About 95% of the PIP implants were done by private clinics, for breast augmentation. Many of these women are seeking urgent appointments with their implanting surgeon.
It is worth repeating that no medical organisation has found any increased cancer risk from the PIP implants compared to other devices. The authorities in France have recommended they be removed as a precaution, and not as a matter of urgency.
Andrew Lansley has given another clear indication that ministers are going to stick to their original advice that the implants do not pose a safety risk.
He denied pre-empting the findings of the expert committee - due on Friday - but said that there was still no evidence to suggest that routine removal of the implants was warranted.
If ministers maintain their position it means that women whose implants are not causing obvious problems would have to pay if they want them removed.
- Published4 January 2012

- Published10 December 2013
