NICE releases new pain relief guidelines
- Published
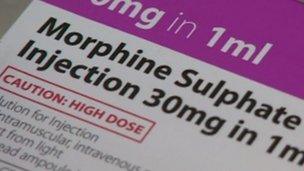
Morphine is one of several powerful painkillers known as opioids
Many patients with advanced cancer and other debilitating conditions are being "under-treated" for their pain, <link> <caption>new guidance from the health watchdog</caption> <url href="http://www.nice.org.uk/CG140" platform="highweb"/> </link> says.
NICE wants doctors in England and Wales to make more use of morphine and other strong opioids - the only adequate pain relief source for many patients.
The guidelines recommend doctors discuss patients' concerns.
These may include addiction, tolerance, side-effects and fears that treatment implies the final stage of life.
The guidance deals with five opioids: morphine, diamorphine (heroin), buprenorphine, fentanyl and oxycodone. They come either from the opium poppy or are synthetically produced versions.
NICE - the National Institute for Clinical Excellence - says "misinterpretations and misunderstanding" have surrounded the use of strong opioids for decades, which has resulted in errors "causing under-dosing and avoidable pain, or overdosing and distressing adverse effects".
There is also the legacy of Dr Harold Shipman who used diamorphine to murder his victims. It has made many doctors wary of prescribing strong opioids.
NICE says the aim is to improve both pain management and patient safety.
Mike Bennett, St Gemma's professor of palliative medicine at the University of Leeds, said: "Almost half of patients with advanced cancer are under-treated for their pain, largely because clinicians are reluctant to use strong opioids."
Prof Bennett said the issue also applied to the late stages of other conditions such as heart failure and neurological disorders.
In a <link> <caption> summary of the guidance</caption> <url href="http://www.bmj.com/content/344/bmj.e2806.full" platform="highweb"/> </link> in the British Medical Journal, he said doctors should address patients' concerns and reassure them that addiction is "very rare".
Doctors are also told to advise patients about side-effects, including constipation, which can be treated with laxatives.
Dr Damien Longson, Chair of the NICE Guideline Development Group said: "People worry they can become addicted, particularly if opioids are prescribed over an extended period of time. This guideline puts a strong emphasis on good communication between healthcare professionals and patients, which is key to ensuring any worries or uncertainties are addressed with timely and accurate information."
Dr Fiona Hicks, chairwoman of the Royal College of Physicians' recent working party on <link> <caption>improving end-of-life care</caption> <url href="http://www.rcplondon.ac.uk/resources/improving-end-life-care-professional-development-physicians" platform="highweb"/> </link> , said she welcomed the new NICE guidelines with its "emphasis on strong communication with patients, including how to help patients cope with both taking opioids and deal with the side-effects."
Sarah Wootton, chief executive of Compassion in Dying, said: "This guideline will support healthcare professionals in providing good end-of-life care across all settings, and will help to ensure that many people have what they consider to be a good death with their pain properly managed."
- Published23 May 2012