Morphine and pain control
- Published
- comments
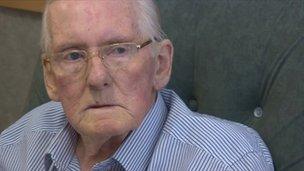
Daniel Hopkins controls his pain with morphine tablets
Daniel Hopkins was told six weeks ago that he has advanced lung cancer.
The 85-year-old from Leeds knows his time left is limited, but he has also had to cope with terrible pain from the cancer, which had spread to his spine.
Treatment with morphine has changed that. He is delighted with his care at St Gemma's Hospice in Leeds, and hoping to go home soon.
He told me: "On a scale of one to ten, the pain was off the top - it was excruciating. Now, I don't have any pain at all. It's marvellous."
Those views are echoed by another patient with advanced cancer at St Gemma's, who is also planning to return home this week.
Anne Jarvis has head and neck cancer and has had her voice-box removed. She is treated with a slow-release opioid patch.
"My pain was totally debilitating and it made it impossible to think straight. I didn't realise it was possible that medicines existed which could relieve that level of pain. They have turned my life around."
Both are cancer patients but opioids are equally needed to help patients with a range of other debilitating conditions such as heart failure, kidney and respiratory illness and neurodegenerative disorders.
New guidance for England and Wales from the health watchdog NICE makes it clear that pain is being hugely under-treated. It wants doctors to prescribe opioids, like morphine, more often. The guidance says that these powerful medicines are often the only means of controlling pain. I have written more about the guidelines here.
Mike Bennett, St Gemma's professor of palliative medicine at the University of Leeds, said both doctors and patients needed reassurance about opioids. He said: "Many doctors share concerns that patients will become addicted, which is rare."

Natalie Laine says despite great nursing care her husband's death was not peaceful
The University of Leeds and St Gemma's Hospice have begun a support programme for patients starting opioid treatment, which will monitor and manage symptoms.
Reading the guidance and research in the British Medical Journal,, external I was amazed at the apparent scale of under-treatment.
It would appear nearly half of all patients with advanced cancer do not have adequate pain control in addition to others with chronic debilitating conditions.
Natalie Laine's husband Mark died from motor neurone disease three years ago at the age of just 32.
He had been on opioids for several months. She says he was very worried about becoming addicted as he knew he would need higher doses as his disease progressed.
Despite excellent nursing care, Mrs Laine says her husband had a terrible end. "He wanted to be out of it at the end and was extremely anxious. He was begging me for help but there was nothing I could do. Stronger opioids would have made a big difference and dealt as much with his anxiety as his pain."
The NICE guidance is not specifically about end-of-life care but rather patients living day-to-day with chronic pain. Nonetheless it will be another factor which will inform the debate about care for the dying.
My television report on this issue is here - just click on the picture below. My thanks to all those patients and medical staff who gave up their time to enable me to report on this important issue.
Many patients with advanced cancer and other debilitating conditions are being "under-treated" for their pain
- Published23 May 2012