More weight loss operations for diabetes
- Published
- comments

An expansion of weight loss surgery in England is being proposed to tackle an epidemic of type 2 diabetes.
New draft guidelines from the National Institute of Health and Care Excellence (NICE) aim to reduce debilitating complications.
Diabetes UK estimates 850,000 people could be eligible for surgery, but NICE expects it to be tens of thousands.
Type 2 diabetes is closely linked to lifestyle and obesity.
Wales and Northern Ireland are not bound by the guidance, but do tend to follow them closely.
The inability to control blood sugar levels can result in blindness, amputations and nerve damage.
A mounting body of evidence suggests a gastric bypass improves symptoms in around 60% of patients.
Around a tenth of NHS budgets, external is spent on diabetes.
The surgery can cost between £3,000 and £15,000 and the move by NICE has raised concerns that the NHS will not be able to afford the treatment, even if there are savings in the longer term.
Current guidance says surgery is an option for people with a BMI above 35 who have other health conditions.

What is bariatric surgery?
Bariatric surgery, also known as weight loss surgery, is used as a last resort to treat people who are dangerously obese and carrying an excessive amount of body fat.
This type of surgery is only available on the NHS to treat people with potentially life-threatening obesity when other treatments have not worked.
Around 8,000 people a year are currently receiving the treatment.
The two most common types of weight loss surgery are:
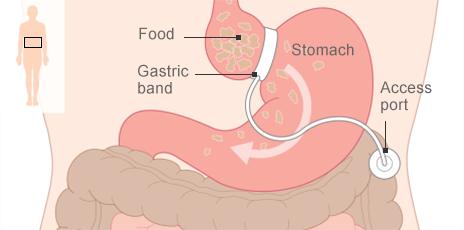
Gastric band, where a band is used to reduce the size of the stomach so a smaller amount of food is required to make someone feel full
Gastric bypass, where the digestive system is re-routed past most of the stomach so less food is digested to make someone feel full

The update in guidance strengthens the focus on those with type 2 diabetes.
It explicitly states that people who have been diagnosed in the past decade and have a BMI over 35 should be assessed for surgery.
The guidelines also suggests doctors should consider those with a BMI of 30 or more on a case-by-case basis.
It means a man who is 6ft (1.83m) tall and weighs 18st 6lb (117kg) would be sent for an assessment, and doctors would be expected to consider sending a 5ft 5in (1.65m) woman, weighing 12st 10lb (80.7kg), as well.
Diabetes UK says around 460,000 people will meet the criteria for an automatic assessment under the guidance.
But the total jumps nearer to 850,000 when those with a BMI of 30 are also considered, it says.
Caroline Merricks, who has type 2 diabetes: ''Bypass surgery would help to prevent a lot more (problems) in the long run''
The figures may be even higher as those of Asian descent should be considered at lower, but unspecified, BMIs.
But NICE's Prof Mark Baker, who drafted the guidelines, said it was "ridiculous" to think so many people would be operated on.
He told the BBC's website: "The first line of attack will be diet and exercise and we would expect clinicians to consider the risks and benefits of surgery for patients."
He said some would not be operated on because of age, concluding: "It would be between 5,000 and 20,000 operations a year, but we haven't done the modelling."
And speaking to the Today programme, he said evidence showed that "relatively early bariatric surgery in the course of [overweight people's] disease can make their diabetes much easier to manage, and in a proportion of cases actually reverse the diagnosis".

Obesity statistics

One in four adults in England are obese
A further 42% of men are classed as overweight
The figure for women is 32%
A BMI of 30-35 cuts life expectancy by up to four years
A BMI of 40 or more cuts life expectancy by up to 10 years
Obesity costs the NHS £5.1bn every year
Source: National Institute of Health and Care Excellence

Simon O'Neill from Diabetes UK said bariatric surgery should only be considered as a "last resort".
And Baroness Barbara Young, the charity's chief executive, told the BBC: "Give me the 5,000 quid that you would spend on an operation and put it into a weight reduction programme earlier on and we could win."
Tam Fry, from the National Obesity Forum, also told the BBC: "A considerable number of people who have had diabetes for some time and have been receiving medication will see a way out which has been sanctioned by NICE and they'll say that's for me.
"But the problem is the health service is going to say, 'No we're out of money, you can't have it', and that's going to create great friction."
James Halstead, a bariatric surgeon at Leeds Nuffield hospital, said recent data showed that the number of NHS-funded bariatric surgical procedures in the UK was falling, not rising.
"It's falling from such an incredibly low baseline level of around 8,000 cases annually that the idea that one can deal with 900,000 people in the next three years with this avenue alone is nonsensical," he said.

Analysis
By Hugh Pym, Health editor, BBC News

More people would be considered for bariatric surgery under the plans
As with so many policy decisions its all about costs and benefits.
NICE is insistent that the cost of bariatric surgery is more than outweighed by what might have been necessary to care for deteriorating health, perhaps running to hundreds of thousands of pounds, over a patient's lifetime.
But the proposal will potentially more than double the number of operations carried out in England.
Patient awareness of the procedure is growing.
It is another example of a demand pressure on the NHS Budget.
A growing population and the increasing needs of the elderly are creating stresses and strains for health service finances.
In the case of obesity, many experts are stressing that the answer is prevention and education and that surgery on the NHS is no long term solution.

Low calorie diet
Meanwhile, the same guidance also says people should not be put on extreme diets to help them lose weight.
NICE acknowledges the diets have become increasingly popular, but warns they do not keep weight off in the long-term.
A very low-calorie diet consists of fewer than 800 calories a day. The normal level advised for an average man is 2,500 calories and for a woman it is 2,000.
Prof Baker earlier said new draft guidance recommended low calorie diets should not be used routinely for the obese.

The diets can still be used in the short-term, for a maximum of 12 weeks, for rapid weight loss before hip or knee replacement surgery or to meet criteria for fertility treatment.
The guidance states that "regaining weight is likely" but that is not down to either "their own or their clinician's failure".
Prof Baker told the Today programme: "The mainstay of weight reduction in people who are obese, whether they have diabetes or not, continues to be diet and exercise,"
"But for some people, whose lives are threatened by the fact that they have diabetes, can be transformed if they are offered they are offered bariatric surgery earlier than our current guidance would allow".
- Published28 May 2014

- Published16 April 2012

- Published3 January 2014
