Antibiotic resistance rise continues
- Published

Antibiotic prescriptions and cases of resistant bacteria in England have continued to soar despite dire warnings and campaigns, figures show.
Public Health England found a 6% increase in prescriptions between 2010 and 2013 and warned that up to half may be "inappropriate".
It found a link between areas of high prescribing and resistant bacteria.
Experts said the report showed we were "squandering an unbelievably precious resource".
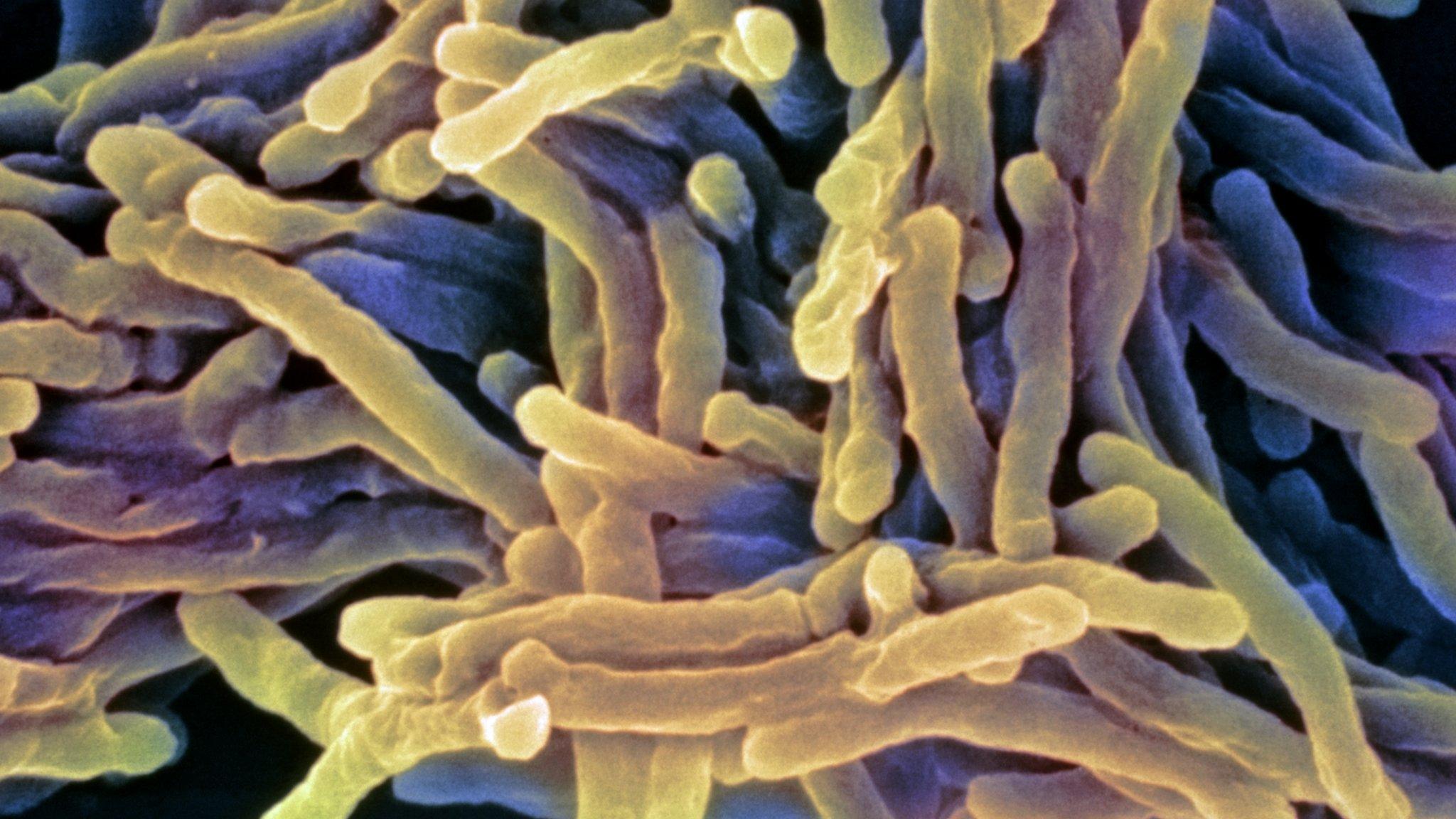
Antibiotics have been one of the greatest breakthroughs in medicine and have saved millions of lives. But there is growing concern that overuse is making them less effective as bacteria develop resistance.
Prime Minister David Cameron has warned the world will be "cast back into the dark ages of medicine" unless action is taken.
The chief medical officer, Prof Dame Sally Davies, has warned of apocalyptic scenarios including routine infections becoming deadly once again.
Widespread variation
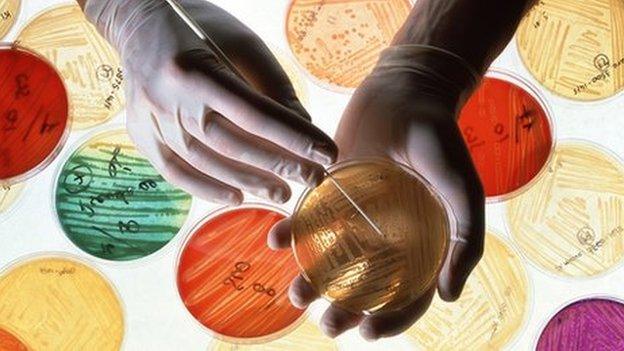
Public Health England has, for the first time, brought together the data on all antibiotic prescribing in England whether in GPs' surgeries, hospitals or dentists.
They have recorded the number of "defined daily doses" of antibiotics prescribed between 2010 and 2013.
In that time prescriptions increased by 6% from 25.9 to 27.4 doses per 1,000 people per day.
There was also a 12% increase in the number of resistant E.coli infections in the blood.
There was widespread variation across the country.
Doctors in Merseyside are prescribing 30.4 defined daily doses per 1,000 people compared with just 22.8 in the Thames Valley region.

Dr Susan Hopkins, from Public Health England, said: "We know that less than 1% of bacteria are extremely multi-drug resistant at the moment, that means resistant to pretty much all the antibiotics we have available to us.
"But in countries like India they are approaching 10% to 20% of individuals they are not able to treat effectively with the antibiotics."
She said England could be heading that way if antibiotics were not used more intelligently.
She argued that giving prescriptions, which could be used only if symptoms became worse in several days' time, would reduce antibiotic use.
And she called for doctors in hospitals to review whether patients needed to stay on antibiotics every day.
'Disappointing'
Prof Laura Piddock, from the group Antibiotic Action, told the BBC: "It is disappointing that antibiotic use and resistance is still increasing, but it's not surprising.
"We have to make it easier for doctors to use antibiotics more wisely when the pressures in the NHS are great and it is really hard for doctors to take on every single guideline."
In the very last year of the study the number of GP prescriptions did start to fall. However, there is concern this is just moving prescribing to other areas of the health service.
Prof Kevin Kerr, the director of infection prevention and control at Harrogate District Hospital, commented: "This is a very important report, which provides yet more evidence that we as a society are squandering an unbelievably precious resource.
"Resistance to antibiotics is rising inexorably and unless we face up to the seriousness of this problem now, the tide of multi-resistant superbugs, which at the moment is lapping around our ankles will rise even further."
Prof John Watson, deputy chief medical officer at the Department of Health, said: "Antimicrobial resistance is one of the biggest threats to health security facing the world today and everybody must take action."
- Published19 November 2015
- Published24 January 2013
- Published2 July 2014
- Published11 March 2013

- Published30 April 2014