NHS needs extra cash and overhaul, say health bosses
- Published
Simon Stevens, the head of NHS England, has suggested a range of measures, including creating larger GP practices
Drastic changes to services and extra money are needed if the NHS in England is not to suffer, health bosses say.
A five-year plan for the NHS - unveiled by six national bodies - once again highlighted an annual £30bn shortfall would open up in the next Parliament.
It said changes, such as GP practices offering hospital services, would help to plug a large chunk of the gap.
But health chiefs said the NHS would still need above-inflation rises of 1.5% over the coming years.
That works out at an extra £8bn a year above inflation by 2020.
The current budget stands at £100bn a year, but all the political parties have already started talking about what they would do in the next Parliament.
Health Secretary Jeremy Hunt said difficult decisions needed to be taken, but added the Conservatives were committed to "protecting and increasing" funding in real terms.
"A strong NHS needs a strong economy, then it is possible to increase spending this report calls for."
£100bn
NHS England budget for 2014-15
£30bn
Shortfall predicted by 2020
-
That could fund 100 hospitals
-
New ways of working could save £22bn
-
But NHS still needs an extra £8bn
Labour's shadow health secretary Andy Burnham said some of the proposals were ideas Labour had already suggested.
"We've have found an extra £2.5bn for the NHS, we've said that the NHS will be our priority in the next Parliament, and alongside that, we're saying that the time has come to bring social care into the NHS."
The Liberal Democrats have said they will make sure the budget rises above inflation.
The five-year plan - called the NHS Forward View - also said the future of the health service depended on it becoming more efficient.
To achieve this, it called for a rethink about the way services were delivered.
It put forward a range of models - although it stressed it was up to each local area to decide which ones to adopt.
These include:
Large GP practices to employ hospital doctors to provide extra services, including diagnostics, chemotherapy and hospital outpatient appointments
In areas where GP services are under strain, hospitals could be encouraged to open their own surgeries
Smaller hospitals to work as part of larger chains, sharing back-office and management services
Larger hospitals to open franchises at smaller sites, as Moorfields Eye Hospital has done in London
Hospitals to provide care direct to care homes to prevent emergency admissions
Volunteers could be encouraged to get more involved, by offering council-tax discounts
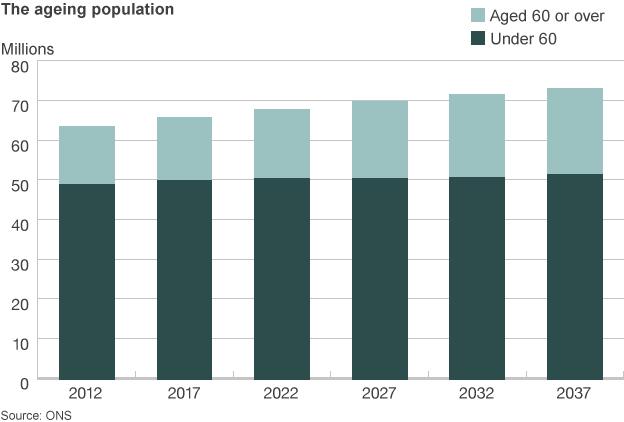
Many of these measures are designed to curb the rise in hospital admissions and the impact of the ageing population - the source of most pressure in the health service.

Case study: Working with care homes
Nurses and doctors from Airedale Hospital in West Yorkshire have set up video link-ups with local care homes.
It allows consultations to take place with residents on everything from cuts and bumps to diabetes management.
Emergency admissions from these homes have reduced by 35% and A&E attendances by 53%.

But the report - produced by NHS England, Public Health England, the regulator Monitor, the NHS Trust Development Authority, Care Quality Commission and Health Education England - also said more needed to be done to reduce obesity, smoking and drinking rates.
It suggested employers should be encouraged to incentivise their staff to become healthier by taking steps such as offering them shopping vouchers for healthy behaviour.
Meanwhile, councils could play their part by using their powers in areas such as planning and licensing to limit the opening of junk food outlets and the sale of cheap high-strength alcohol.
Simon Stevens, chief executive of NHS England, the lead body for Forward View, said the NHS was at a "crossroads".
NHS England chief executive Simon Stevens: NHS "must fundamentally change"
"It is perfectly possible to improve and sustain the NHS over the next five years in a way that the public and patients want. But the NHS needs to change substantially."
He said if the health service did not improve, the "consequences for patients will be severe" in terms of what could be done to ensure patients received the best care in areas such as cancer and heart disease.
But he added there was no reason why a tax-funded NHS would not continue if the plans outlined were followed.
'Close the gap'
Health minister Norman Lamb welcomed the report, saying it was "really imaginative thinking".
"I think this combined case of more investment but also change... is absolutely the right message."
The Liberal Democrat minister said his party wanted to "reopen" spending plans for 2015/16, saying "the NHS needs more money next year". He said it would be "our top priority" for the Autumn Statement.

Case study: The GP super-practice
Whitstable Medical Practice, in Kent, is one of the new super-practices that are being developed. It offers the traditional GP services alongside a host of services more associated with hospitals.
It operates out of three sites and employs nearly 150 staff, providing care for 34,000 people.
It runs maternity services, a minor injury unit with X-ray facilities and dedicated diabetes, heart disease and asthma clinics as well as diagnostics and minor surgery.

Nigel Edwards, the chief executive of the Nuffield Trust think tank, said: "This report makes crystal clear that the NHS cannot continue with 'business as usual' if it is to meet the needs of a diverse and ageing population."
Royal College of Nursing general secretary Peter Carter called the report "rigorous and realistic".
- Published22 October 2014

- Published23 October 2014
- Published23 October 2014
- Published23 October 2014

- Published19 September 2014

- Published10 July 2014

- Published7 July 2014

- Published29 June 2014

- Published18 June 2014

- Published1 April 2014
