A&E waiting in England worst for a decade
- Published

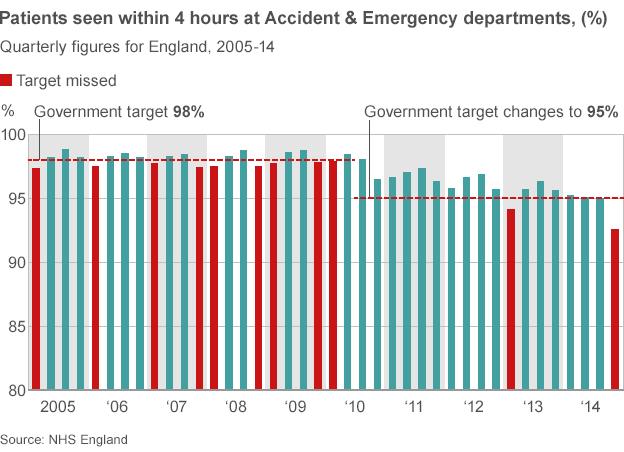
The NHS in England has missed its four-hour A&E waiting time target with performance dropping to its lowest level for a decade, figures show.
From October to December 92.6% of patients were seen in four hours - below the 95% target.
The performance is the worst quarterly result since the target was introduced at the end of 2004.
The rest of the UK is also missing the target and a number of hospitals have declared "major incidents" recently.
This signifies they are facing exceptional pressures and triggers extra staff being called in and other steps, including cancelling non-emergency care, such as routine operations.
Health Secretary Jeremy Hunt admitted meeting the A&E standard was proving tough, but pointed out that England has some of the toughest targets in the world.

Get involved on:
"Targets matter but not at any cost. The priority is to treat people with dignity and respect."
But Shadow Health Secretary Andy Burnham said patients were being exposed to "an unacceptable levels of risk".
"This crisis in A&E has its roots in the government's cuts to social care and GP access and its disastrous decision to throw the NHS into the chaos of reorganisation."
'Intolerable pressure'
It is the second time the target - which measures the point from arrival to being discharged, admitted to hospital or transferred elsewhere - has been missed under the coalition.
In the first three months of 2013 94.1% of patients were seen in four hours.
Meeting the target has proved particularly tough since the end of the summer.
The target has been missed on a weekly basis - England provides these figures along with the quarterly statistics - every week except one since the end of August.
Jeremy Hunt: "It is a very tough time on the front line at the moment"

Analysis: What is a major incident?
If a hospital declares a major incident or internal incident, it is a sign that things have got exceptionally busy and special measures are need to cope.
This can happen in winter when demands are high, but also at other times, for example if there is a major road accident. The declaration allows hospital bosses to call in extra staff to help them cope. But it is also worth noting that some hospitals may not necessarily go public with their problems. You can be sure that there are more sites under intense pressure than the numbers officially on alert.
What is important is what steps they take in terms of restricting the flow of patients into the hospital. One of the first measures is to start postponing routine activity, such as knee and hip operations or outpatient appointments. This is not uncommon - and is likely to be happening at a significant number of sites at the moment.
More unusual is diverting ambulances so no emergency patients arrive. In effect, that closes the hospital. However, this is only used as a last resort as it increases demands on nearby sites.

However, the performance in England is still better than elsewhere in the UK. The data in the other nations lags a bit behind England.
In Wales the data from November shows just 83.8% of patients were seen in time.
Northern Ireland is performing even worse - just over 80% of patients were seen within four hours in November.
Scotland has a slightly tougher waiting time target - 98% of patients should be seen in four hours - but in September 93.5% were.
Comparing the September figures for England and Scotland shows England was performing slightly better in that month.
It means according to latest data all parts of the UK are missing the A&E waiting time target.
Labour's Andy Burnham said: "This crisis in A&E has its roots in the Government's cuts to social care and GP access and its disastrous decision to throw the NHS into the chaos of reorganisation."
Dr Cliff Mann, of the College of Emergency Medicine, warned hospitals were reaching a "tipping point".
He said part of the reason was the NHS non-emergency line 111 advising an increasing proportion of people to seek emergency care.
Dr Mann said: "My concern is the daily intolerable pressure is starting to have an effect on staff - they are more likely to become sick, become unable to work, burn out and choose to go into other professions. That means it is not a sustainable situation".
Royal College of Nursing general secretary Peter Carter said: "These figures show what patients and staff already know - A&E departments are constantly running at full capacity. Patients and hardworking staff are being let down by a system which is in crisis."
Labour's Andy Burnham blamed what he described as the crisis facing the NHS on the government's "severe cuts to social care"
Dr Mark Porter, of the British Medical Association, added hospitals were facing "unprecedented levels of demand".
"Staff are working flat out but the system is struggling to cope with the sheer number of patients coming through the door. Growing pressure on services throughout the year means hospitals have no spare capacity to deal with the winter spike in demand."

How the UK has prepared for winter
In England an extra £700m has been set aside to help the NHS. This is paying for the equivalent of 1,000 extra doctors, 2,000 nurses and 2,000 community staff, including social workers and physios.
Ministers in Scotland have announced a total of £28.2m for the NHS to increase capacity and improve the way patients are discharged during winter.
In Wales the NHS has been given an extra £200m for this year. The money is for the whole health service, but ministers say it will help relieve pressure in the coming months.
Ministers in Northern Ireland have released an additional £5m for both hospitals and the community, including ambulance liaison officers to speed up handovers between paramedics and A&E teams.
- Published7 January 2015

- Published6 January 2015
- Published6 January 2015

- Published6 January 2015

- Published6 January 2015
- Published5 January 2015
- Published19 December 2014

- Published7 January 2015

- Published12 December 2014

- Published18 June 2014

- Published17 March 2014
