Doctors 'should snoop on antibiotic prescribing'
- Published

Doctors should snoop on their colleagues to ensure they are not prescribing too many antibiotics, the NHS in England suggests.
It is one of the National Institute for Health and Care Excellence (NICE) recommendations to avert the growing problem of antimicrobial resistance.
Its draft guidelines also say doctors need to say no to pushy patients.
They add that it is time to "turn this tanker around" after years of failed policies to cut antibiotic use.
Figures show a 6% increase in antibiotic prescriptions between 2010 and 2013, with half deemed "inappropriate".
That is despite repeated warnings that one of doctors' best weapons is about to be ripped out of their hands by the rise of resistant bugs.
As well as untreatable infections, surgery, chemotherapy and organ transplants become impossible without the support of antibiotics.
"Antibiotic use has gone up and up and up each year despite a number of initiatives to damp down on their use," said Prof Mike Baker, the director of the centre for clinical practice at NICE.
The organisation, which establishes best practice for the NHS, has prepared new guidelines for how the drugs are used.

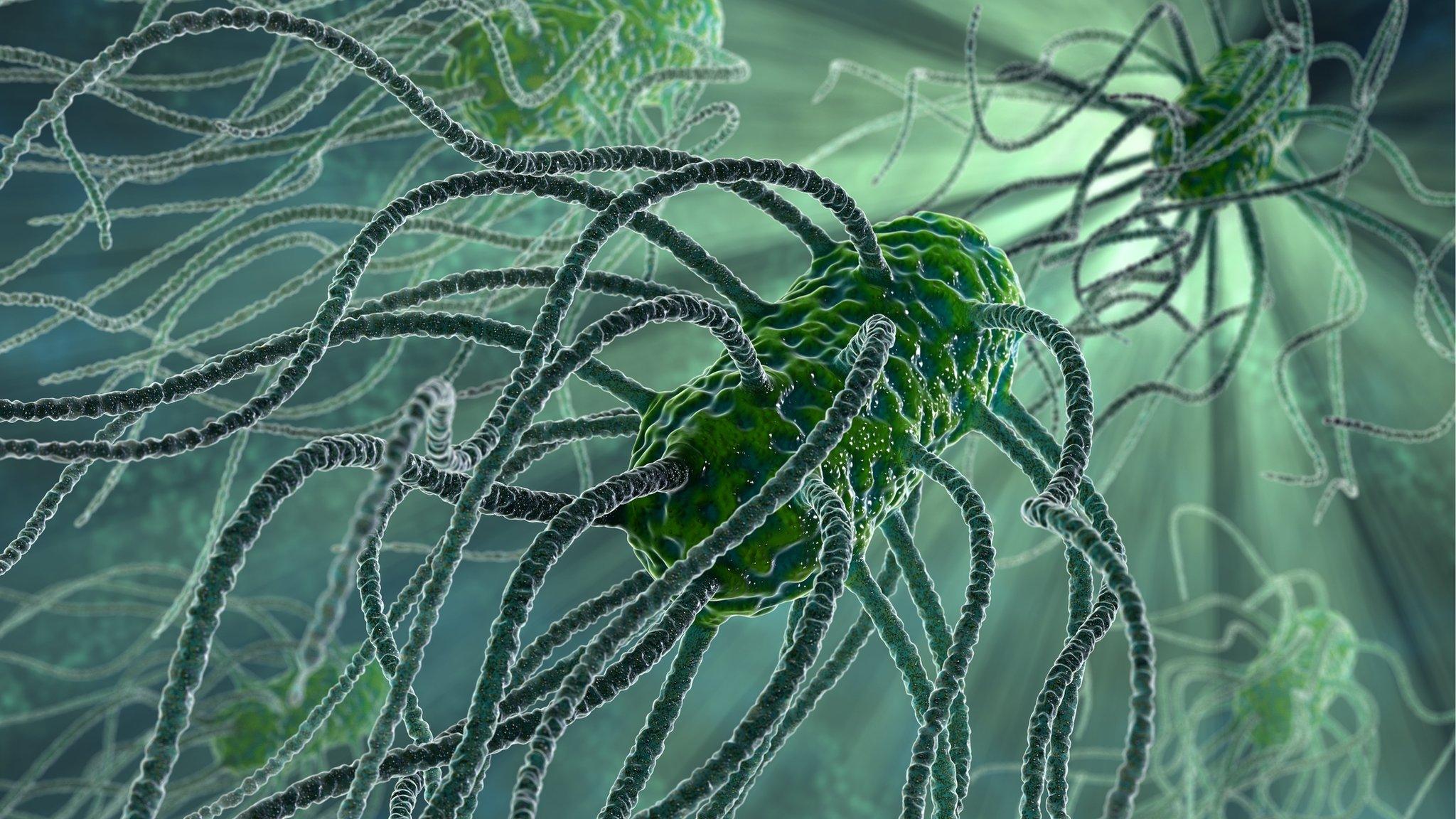
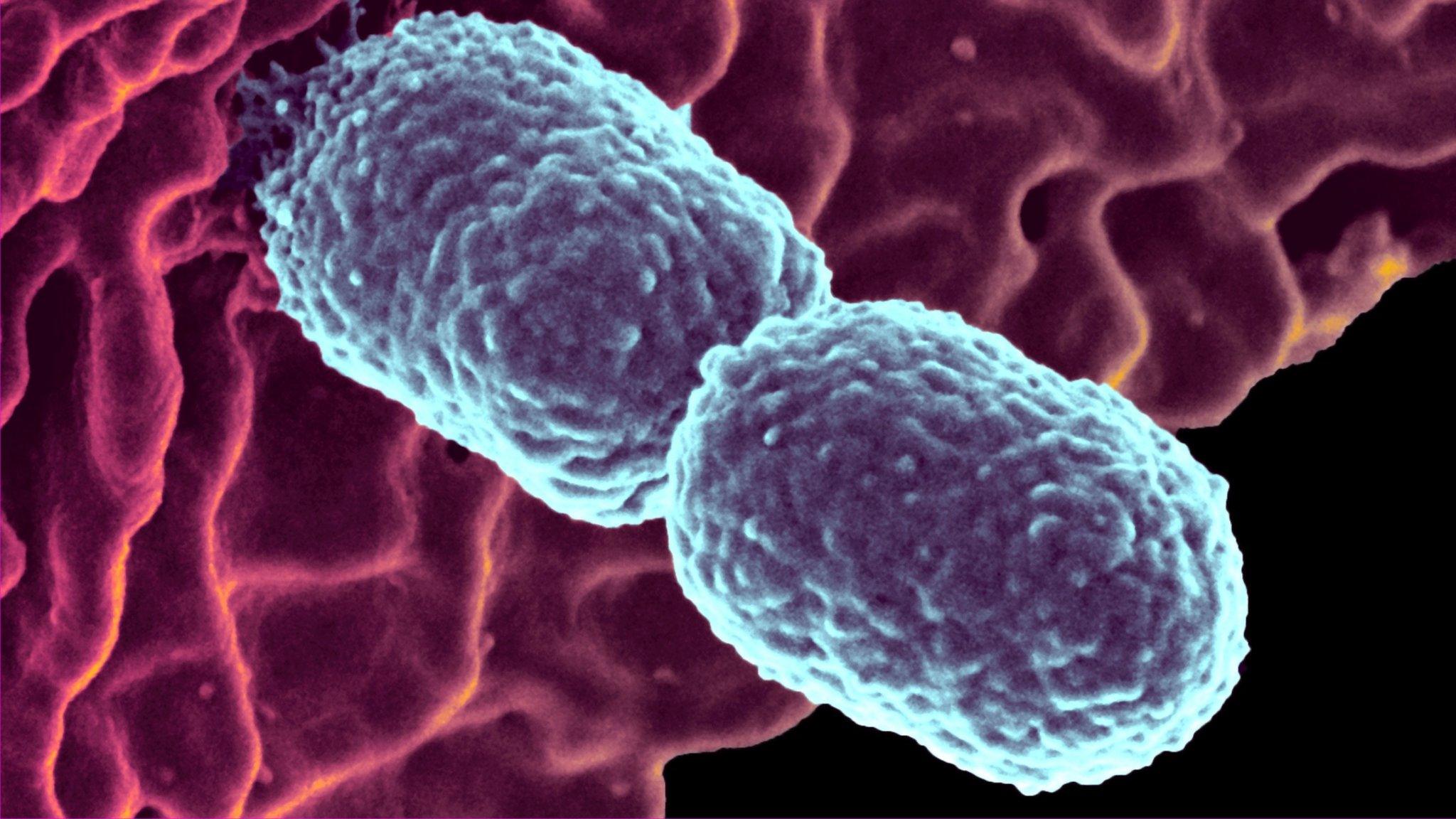
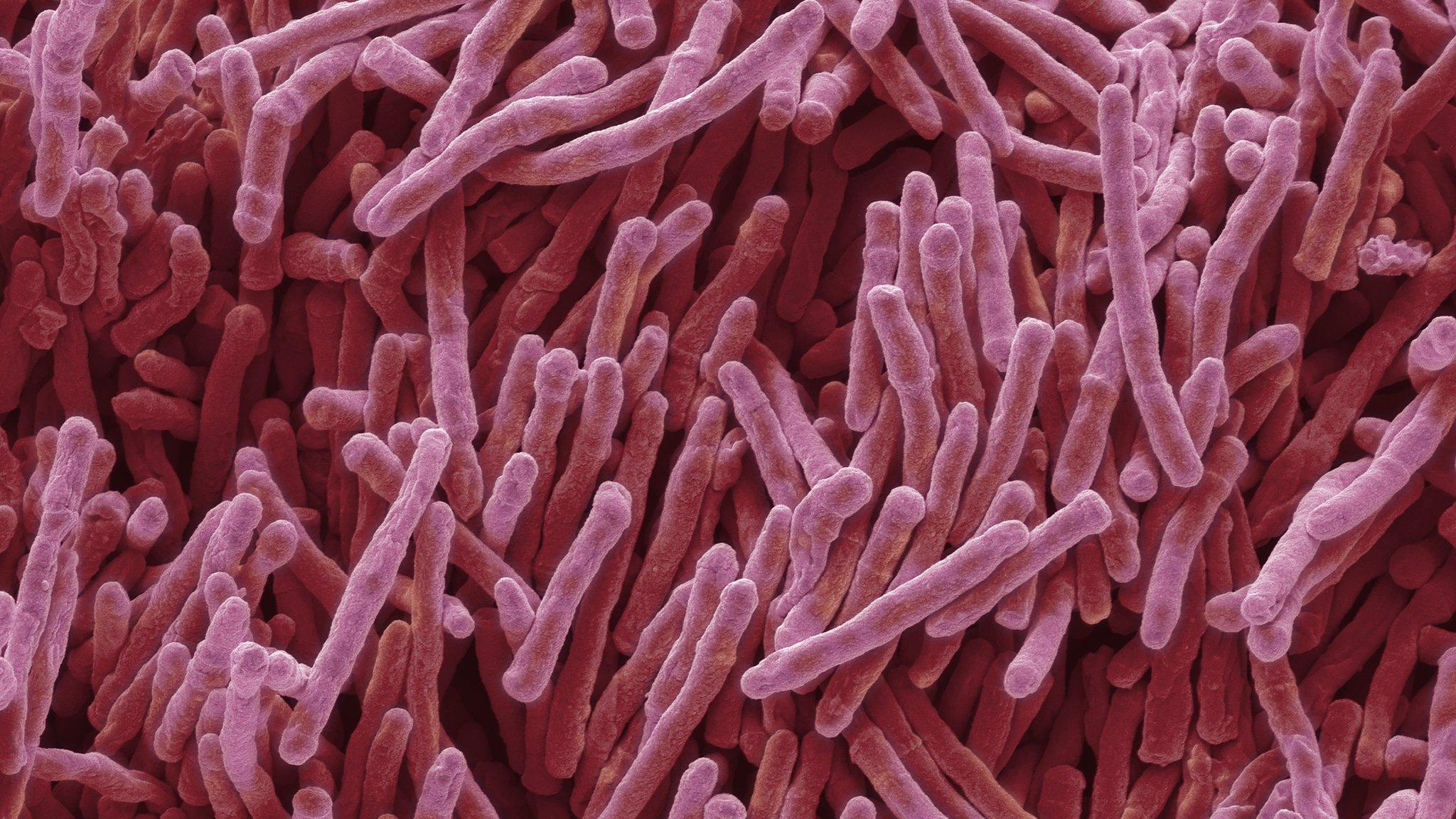
Scientists say more and more cases of drug resistance are being reported
One proposal is for doctors to keep tabs on their colleagues.
Prof Baker told the BBC News website: "I think peer pressure has to be a part of any strategy to reduce antimicrobial use.
"Health professionals should question the practices of colleagues when they are not in line with local and national guidelines.
"We have to turn this tanker around."
'Watchful waiting'
The guidelines also say doctors need to be far more comfortable saying no to patients, even those who are insistent on having antibiotics.
"Patient pressure is a real problem and it puts GPs under pressure, and they can be afraid of not prescribing antibiotics even when they know it's wrong."
The suggested rules say doctors should spend more time explaining why antibiotics are unsuitable for many patients.
There should also be wider use of "watchful waiting" when antibiotics are used if the patient's health does not improve.
However, Prof Baker insisted these ideas were not a "blunt instrument" and that doctors needed to "walk a tightrope" as not prescribing antibiotics had the potential to lead to sepsis in some cases.
'Too dependent'
The chief medical officer for England, Prof Dame Sally Davies, responded: "Preserving the effectiveness of the antibiotics we have is absolutely crucial and everybody, including patients, has a role to play.
"We want prescribers to engage with the consultation and give their views on how current practice can be improved."
Dr Maureen Baker, the chairwoman of the Royal College of GPs, said: "Antibiotics have served us well in treating infections for over 60 years, but as a society we have become too dependent on them and they are now seen as a 'catch-all' for every illness and infection.
"GPs can come under enormous pressure from patients to prescribe antibiotics, so we welcome a team approach to ensuring that this is done appropriately and that they are used responsibly.
"It is essential that GPs, their practice teams and pharmacists discuss the alternatives with patients who ask for antibiotics to treat minor illnesses, most of which will get better on their own over time."
- Published10 October 2014
- Published7 January 2015
- Published19 November 2015