Call for $2bn global antibiotic research fund
- Published
- comments

Some bacteria are becoming resistant to our best drugs
The global pharmaceutical industry is being called on to pay for a $2bn (£1.3bn) innovation fund to revitalise research into antibiotics.
In return, there would be guaranteed payments to companies which produced vitally needed new antibiotics.
There are currently very few new antibiotics in development amid a global spread of resistant bacteria.
The proposals are in a report by a UK government-appointed review team headed by economist Jim O'Neill.
Mr O'Neill said: "We need to kick-start drug development to make sure the world has the drugs it needs, to treat infections and to enable modern medicine and surgery to continue as we know it."
He has previously warned that drug-resistant microbes could kill 10 million people a year worldwide by 2050 and cost $100 trillion in lost economic output.
How do antibiotic resistance blockers work?
Resistant strains of bacteria are spreading globally, threatening to make existing drugs ineffective.
A global innovation fund of $2bn over five years would be used to boost funding for "blue-sky" research into drugs and diagnostics - with much of the money going to universities and small biotech companies.
One promising area of research concerns so-called "resistance breakers". These are compounds that work to boost the effectiveness of existing antibiotics - a far less costly approach than attempting to discover entirely new drugs.
Helperby Therapeutics, a spin-out company founded by Prof Anthony Coates, St George's, University of London, has created a resistance breaker that acts against the superbug MRSA.
The compound, known as HT61, will shortly go into clinical trials in India, where it is being developed under licence by Cadila Pharmaceuticals India.
The review team said this kind of research could benefit from the innovation fund and could be the key to making existing drugs last longer.
Mr O'Neill said the big pharmaceutical companies should pay for the fund and look beyond short-term assessments of profit and loss.
Formerly chief economist with the investment bank Goldman Sachs, Mr O'Neill drew parallels between the banking crisis and the looming catastrophe of a world where antibiotics no longer worked.
Innovation funding
He said big pharma needed to act with "enlightened self-interest" because "if it gets really bad, somebody is going to come gunning for these guys just how people came gunning for finance".
Mr O'Neill was speaking to the BBC's Panorama programme, which has spent six months following the work of the review team, filming in India, the US and UK.
Mr O'Neill was appointed last year by Prime Minister David Cameron to head the review into antimicrobial resistance - which already claims an estimated 30,000 lives a year across Europe.
Many large companies have pulled out of antibiotic research.
The report says this is partly due to the uncertain commercial returns for new antibiotics.
Could soil hold the key for new antibiotics?
New drugs are often kept in reserve for years, to preserve their potency, by which time they may be nearing the end of their patent.
After this expires, cheaper generic versions are available.
In order to incentivise drug development, the review team says, there should be lump-sum payments to companies that create proven new antibiotics.
This would break the link between the profitability of a drug and its volume of sales.
The review team predicts its proposals could lead to 15 new antibiotics a decade, of which at least four should be "breakthrough products" targeting the bacterial species of greatest concern.
It estimates the cost of guaranteed payments for these drugs would be $16-37bn over a decade but says this is a small price to pay given that antibiotics are essential to so many aspects of healthcare, from common infections, to surgery and cancer treatment.
US breakthrough

A new drug, effective against tuberculosis and MRSA, should be trialled on patients within two years
It is nearly 30 years since a new class of antibiotics - meaning a group of drugs with an entirely novel action - was introduced.
But this decades-long drought could be over as a result of a breakthrough recently announced by US scientists.
A team at Northeastern University in Boston, Massachusetts, has discovered 25 potential new antibiotics, all of them derived from soil microbes.
One of them, teixobactin, is effective against both tuberculosis and MRSA.
The drug is being developed by NovoBiotic Pharmaceuticals and should go into patient trials within two years.
Prof Kim Lewis, of Northeastern University, who co-founded the company, told Panorama: "We think there could be thousands more antibiotics in the soil, yet to be discovered."
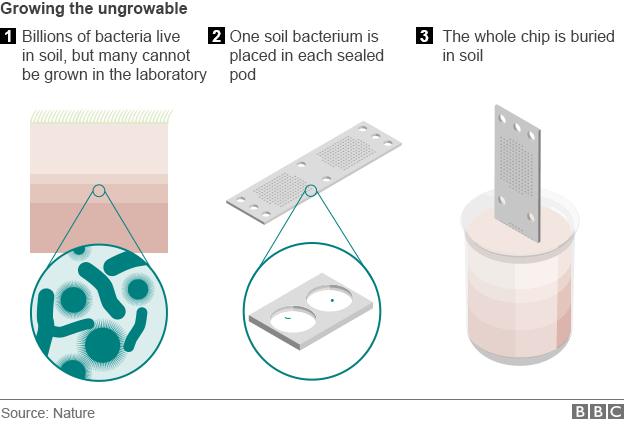
The team at Northeastern University created a device to help them study the bacteria
There are still many uncertainties.
Teixobactin has yet to undergo patient trials, and it is at this stage that many promising drugs fail.
Nor is it effective against bacteria such as E.coli and Klebsiella, which are responsible for a huge proportion of resistant infections.
But the Boston team's discoveries are the type of innovative research many scientists believe essential to ensure we do not run out of effective antibiotics.
Patrick Vallance, GlaxoSmithKline's president of pharmaceutical R&D said that, as one of the few companies still conducting antibiotic research they welcomed the report: "We are very encouraged by the ideas it sets out to modernise the economic model to encourage investment in research and ensure reasonable returns."
Prof Dame Sally Davies, chief medical adviser to the UK government, said: "We have to respond to the challenge of antimicrobial resistance by making sure we secure the necessary antibiotics for generations to come, in order to save millions of lives and billions of pounds."
Panorama: Antibiotic Apocalypse is on Monday 18 May on BBC ONE at 20:30 BST or you can catch up oniPlayer.
- Published11 December 2014
- Published2 July 2014
- Published11 March 2013

- Published19 November 2015