Hospitals given green light to miss waiting time targets
- Published

More than 50 hospitals in England have been given the green light to miss key waiting time targets this year to help ease their financial problems.
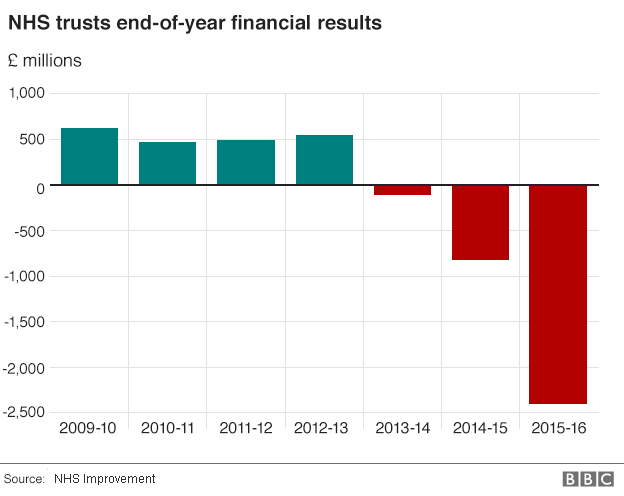
The move is part of a package of measures taken by NHS bosses after hospitals exceeded their budgets by a record amount last year.
Fines for missing targets in A&E, cancer and routine operations have been scrapped altogether.
And a new failure regime is being set up for the worst-performing trusts.
It will see regulators parachute senior managers into the hospitals to help devise plans to get them out of trouble.
Five trusts - Barts Health in London, Croydon Health Services, Maidstone and Tunbridge Wells, Norfolk and Norwich Hospitals and North Bristol - have been placed into the new regime immediately, with another 13 threatened with the prospect.
But the relaxation of rules over waiting times is the most radical element of the announcement made by bosses at the three national bodies that oversee the health service - NHS England and the regulators NHS Improvement and the Care Quality Commission.
Hospitals have been struggling to hit their targets for some time and will now no longer be fined for missing the four-hour A&E target, the 62-day target to get cancer treatment and the 18-week goal for routine operations, such as hip and knee replacements.
Instead, they will have to simply improve on their current performance to get their slice of the extra money being invested in the NHS this year.
Each hospital has been given its own target for improvement and, crucially for some and particularly in regards to A&E, it allows them to get the funding without achieving the official targets by March.
This is the case for 53 out of the 139 trusts running A&E units, five cancer hospitals and three sites doing routine operations.

Targets and fines: How they work
A&E: 95% of patients are meant to be dealt with in four hours. When this is exceeded a fine of £120 per patient is levied. The fines are capped so that when performance drops below 85% no more penalties are imposed.
Routine operations: 92% of patients are meant to start treatment within 18 weeks. When the numbers waiting longer than this exceed that threshold hospitals are fined £400 per patient. Once it drops to 90% the level of the fines are capped.
Cancer: Hospitals are meant to start treatment on patients who receive an urgent referral by a GP within 62 days for 85% of patients. Fines of £1,000 per patient are levied when patients wait longer. There is no cap.

The move was criticised by the Patients Association. Its chief executive Katherine Murphy said: "This is the slippery slope back to the bad old days of never-ending waiting times and uncertainty - with patients left endlessly on A&E trolleys and waiting for life-changing operations. Where is it all going to end?"
Health bosses believe the measures will help the NHS get the deficit down to £250m this year after an overspend of £2.45bn was posted in 2015-16, the highest ever recorded and triple what it was the previous year.
That figure also covered the budgets for mental health units and ambulances, but it was the hospital sector that ran into the most difficulties with nearly nine in 10 ending the year in the red.
NHS England chief executive Simon Stevens said this was a make-or-break period.
"Precisely because the pressures across the NHS are real and growing, we need to use this year both to stabilise finances and kickstart the wider changes everyone can see are needed."
But Nigel Edwards, of the Nuffield Trust think tank, predicted the measures being taken on their own would not be enough.
"My big worry is what happens next. I fear that in order for hospitals to virtually eradicate their deficits the next steps could be a series of brutal service reductions and bed closures - which will shock an unprepared public."
Meanwhile, it has emerged the financial problems in hospitals almost meant the Department of Health failed to balance its budget overall, which could have meant sanctions from the Treasury.
The department managed to cover the overspend by trusts by drawing on surpluses elsewhere in the health service, which meant it finished £210m in surplus on a budget of nearly £115bn.
But this came only after it raided the capital budget, which is set aside for buildings and maintenance, by £950m, and identified £417m of extra income from national insurance receipts which it had failed to declare initially - something officials blamed on an "administrative error".
Auditors said the steps taken this year to balance the books were not sustainable and should be considered a one-off.
- Published15 March 2016
- Published25 February 2016
- Published16 December 2015

- Published9 October 2015
- Published18 June 2014
