Cervical screening 'could save hundreds more lives'
- Published

The lives of hundreds more cervical cancer patients could be saved if all those eligible went for screening, says a study published in the British Journal of Cancer.
Nearly 2,000 women's lives are saved as a result of cervical cancer screening in England each year, the report found, external.
Researchers from Queen Mary University of London said the biggest impact of screening was among women aged 50-64.
Around 800 women die from cervical cancer in England each year.
Cervical cancer screening is offered to women in the UK aged between 25 and 64.
Between 25 and 49, women are invited for screening every three years, and up to the age of 64, every five years.
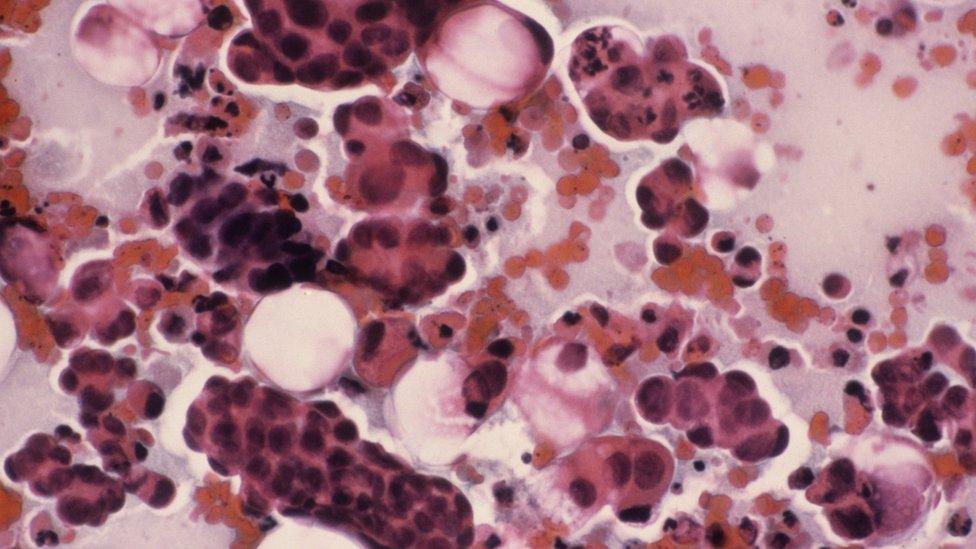
Screening involves a smear test which searches the entrance of the womb for abnormal cells.
This gives doctors a chance to remove tissue that might become cancerous.
11,000 records
The research team analysed the records of more than 11,000 women in England who had been diagnosed with cervical cancer.
The researchers found that 350 extra lives could be saved if all women aged between 25 and 64 were screened regularly.
And if there was no screening among 50 to 64-year-olds, five times more women would die from cervical cancer.
Prof Peter Sasieni, lead researcher based at Queen Mary University of London, said many women were alive and healthy thanks to the screening programme.
"The cervical screening programme already prevents thousands of cancers each year and as it continues to improve, by testing all samples for the human papilloma virus (HPV), even more women are likely to avoid this disease."
Dr Claire Knight, health information manager at Cancer Research UK, recommended that women take up the offer to attend cervical screening when invited.
"It's important to remember that cervical screening is for women without symptoms.
"Women who have any unusual or persistent bleeding, pain, or change in vaginal discharge - even if they've been screened recently and whatever their age - should get it checked out by their GP."
- Published6 September 2016