10 charts that show what’s gone wrong with social care
- Published

Ministers in England have said they are looking for a solution to the problems in social care. That has raised hope that next month's Budget could include measures to tackle what many describe as the crisis facing the sector.
But what exactly has gone wrong? And who's affected?
Social care - organised by councils - is a broad term that covers everything from children's social workers and fostering through to services for disabled adults and the care provided to people in their old age. But some have been affected more than others.

1. Social care spending has stopped rising
Over the years, more and more has been spent on services. The growth in the population, the fact people are living longer and those with disabilities are more likely to survive to an older age are all contributory factors.
But this upward trend in funding has tailed off in England over the past decade.
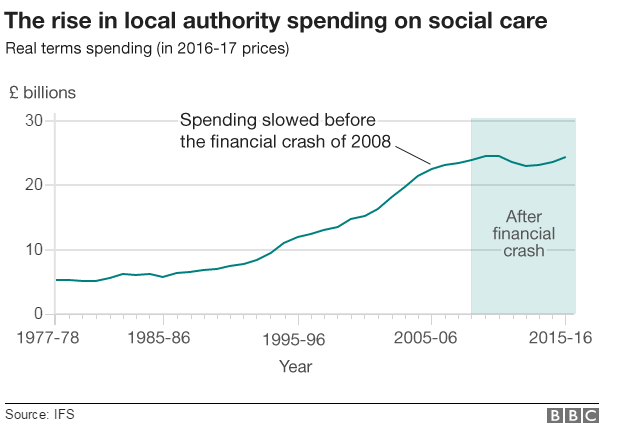
You do not have to look far to find the cause of this. Central government funding for councils was cut by a third during the last parliament.

2. Councils are prioritising care
Councils have tried to protect social care. The proportion of their budget being spent on these services has increased over the years and now well over half of their spending goes on care services.
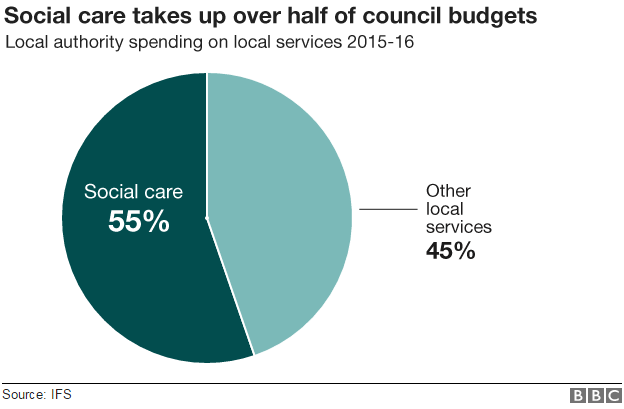
But that, of course, has meant deeper cuts elsewhere - in libraries, leisure centres and refuse collection.

3. The NHS is propping up care
What's more, if you delve further into the figures you can see even this level of spending has been maintained only with a little help from elsewhere.
A third of last year's £24bn budget went on children.
That left just over £16bn for adults. But nearly £2bn of that was thanks to a transfer of money from the NHS into care services, ordered by the government.
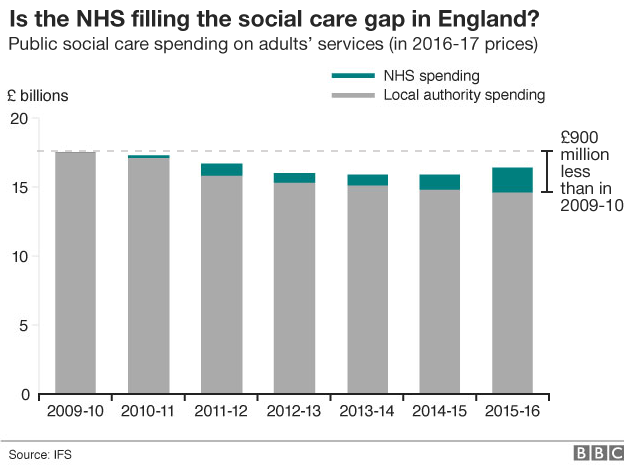
This is a recognition that what happens in social care has a direct impact on the NHS.

4. No care means patients get stranded
If people are not given the support they need in the community, they can end up in hospital.
And if it's not available when they are then ready to be discharged, they can end up stranded on wards - doctors will release frail patients only if they know there are care packages in place in the community.
The number of delays of this sort has nearly doubled in five years.
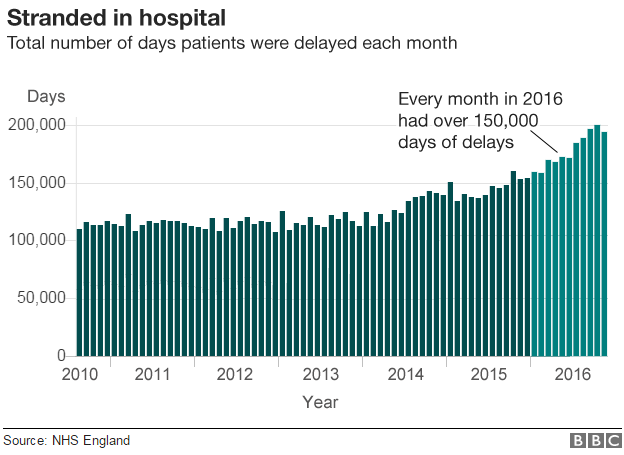
Not all of these delays are down to a lack of social care, but it is the fastest growing reason for them.
And when beds are occupied by patients who cannot leave, it gets more difficult to admit new patients.
That's one of the reasons why we have heard so much about lengthening trolley waits and worsening waiting times in accident and emergency departments in recent months.

5. Councils are looking after fewer older people
This situation is understandable. To make savings, councils have started to ration care, particularly to the elderly, rather than younger adults with disabilities.
The number of older people getting care from councils has fallen by over a quarter between 2008-09 and 2013-14.
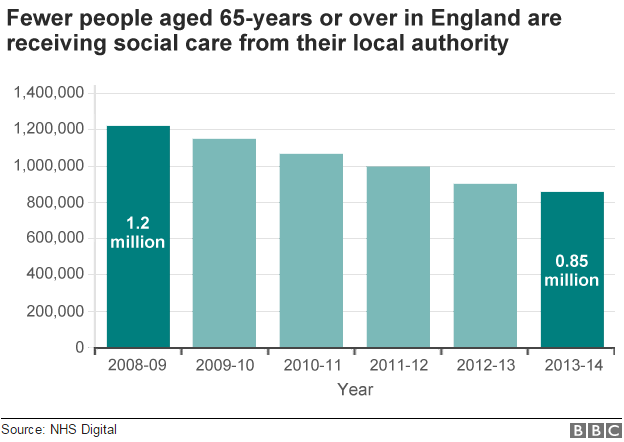
We don't know what has happened since 2014, as the way the data is collected has changed. Although, it's pretty clear there hasn't been a huge turnaround.
Councils agreed to help less than half the older people who approached them for help last year.
What about elsewhere in the UK? Whereas all adult council care in England is means-tested - those with assets of over £23,250 pay the full costs of their care - Wales, Northern Ireland and Scotland have slightly different systems.
In Wales, the cost of help in the home for daily tasks such as washing and dressing is capped at £60 a week, in Northern Ireland it is provided free to the over-75s, and in Scotland personal care is free whether the individual is in their own home or a care home.
Many argue these systems are more generous. That may be so. But all have had to ration services in recent years by restricting access to only the people with the most severe needs.

6. People are being left to fend for themselves
The result of this is that people make their own arrangements. Four in 10 people in care homes pay for themselves.
Others rely on family and friends to look after them. But growing numbers are being left to struggle on with no or little help.
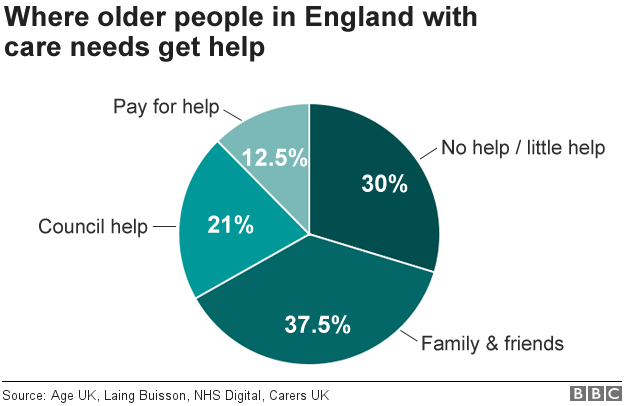
The charity Age UK has been charting this. It estimates the number of those falling into this group has risen by nearly 50% since 2010, to 1.2 million.
These are people who have pretty substantial needs. They cannot wash or dress themselves. They may struggle to go to the toilet. The stories they tell are heart-breaking.

7. Self-funders appear to be subsidising councils
But it's not just individuals who have tales of woe. The companies providing the services - councils tend not to run them in-house - have started voicing concerns.
They report the prices councils are paying are being squeezed so much that they are now making a loss in some areas from local authority work.
The UK Home Care Association has calculated the cost of helping people in their own home is £16.70 an hour, but councils across the UK pay over £2 less than this on average.
Meanwhile, analysts LaingBuisson have calculated that the fees being paid by councils for a care home place are £100 a week less than the true cost.
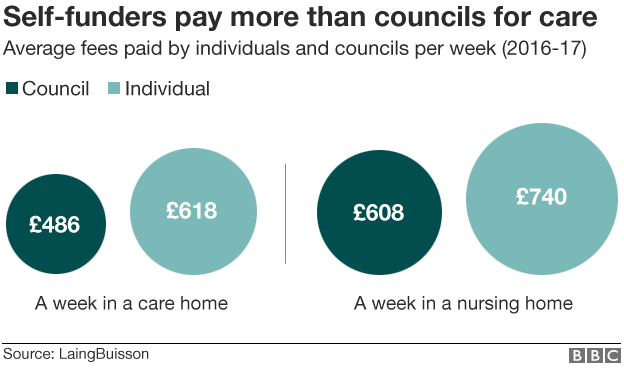
It means the fees for those who pay for themselves are rising to offset the losses from local authority funded residents. In effect, self-funders are subsidising the state sector.
Is this fair? LaingBuisson thinks not. It has called the trend a "hidden care tax".
And these bills can rack up. An estimated one in 10 people faces care costs in excess of £100,000 after the age of 65.

Find out the cost of care in your area

8. The care market could be at risk
There is concern this is destabilising the sector. The Care Quality Commission raised the alarm about this last autumn.
The risk is care companies start to focus on areas where there are more of the high-paying self-funders.
That could create a shortage of places in some areas of the country, as self-funders are more likely to be found in the south of England.

The map of the UK shows self-funders are more likely to be found in care homes in the South East of England
There has not been a big exodus yet, although the number of care and nursing homes operating in England has fallen by over 1,500 in the past six years to 16,500.

9. The population is ageing
So what does the future hold? The population is growing older.
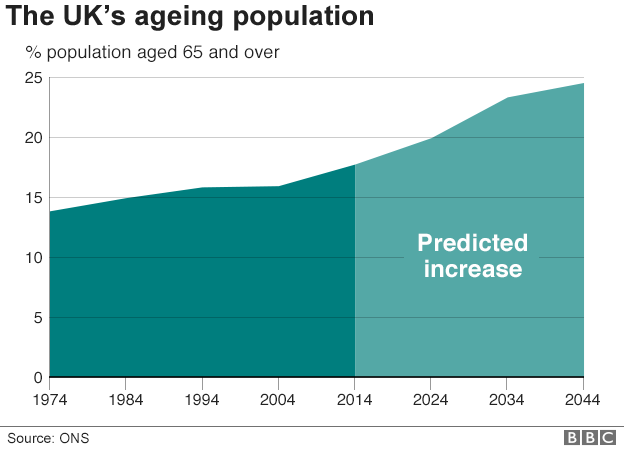
And their needs are getting ever more complex. At the age of 65, one in six people has trouble with daily living - washing, dressing or eating. By 85, half do.

10. Council tax bills are rising to help councils cope
Ministers have already taken steps to relieve the pressure.
The health service and councils are being encouraged to work together on joint projects.
They have also given councils permission to increase council tax to pay for social care.
But there is a limit to how much this will bring in.
This year, councils have been allowed to increase household bills by 2%.
Most have done so, but it is raising less than 3% of what councils plan to spend on adult social care from their own funds, once NHS money has been deducted.
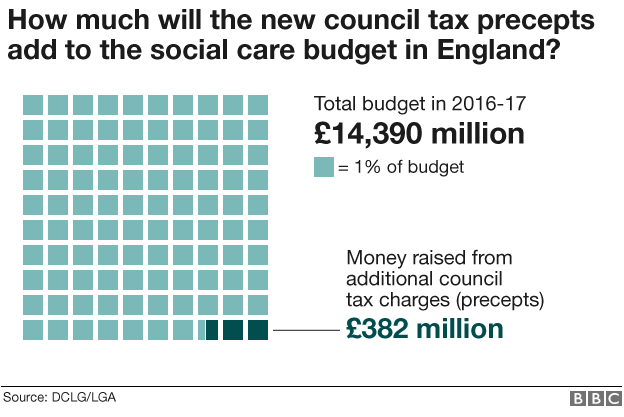
By 2020, the Local Government Association believes, there will be a shortfall of £2.6bn in funding.
It wants more substantial reform - and many in academia, in the health service and in the charity sector agree.
Health Secretary Jeremy Hunt has said this is on the government's agenda. But many have tried to find a solution before and failed.
The social care system was created in 1948 and has hardly changed since.
When Tony Blair came to power, he set up a Royal Commission. But nothing came of it.
Under Gordon Brown's premiership, the idea of a universal care system - where everybody would get a basic level of care - was floated, before it fell victim to the Tories' 2010 "death tax" election campaign warning.
The coalition government proposed a cap on care costs. That was meant to be introduced last year, but has been pushed back until 2020. Many now doubt it will ever see the light of day. And so the social care problem rumbles on.

- Published8 February 2017

- Published8 February 2017

- Published6 January 2017

- Published12 December 2016

- Published13 September 2016













