Cuts to sexual-health services imminent
- Published
Liv from north Norfolk has to travel 25 miles to get to her nearest sexual health clinic
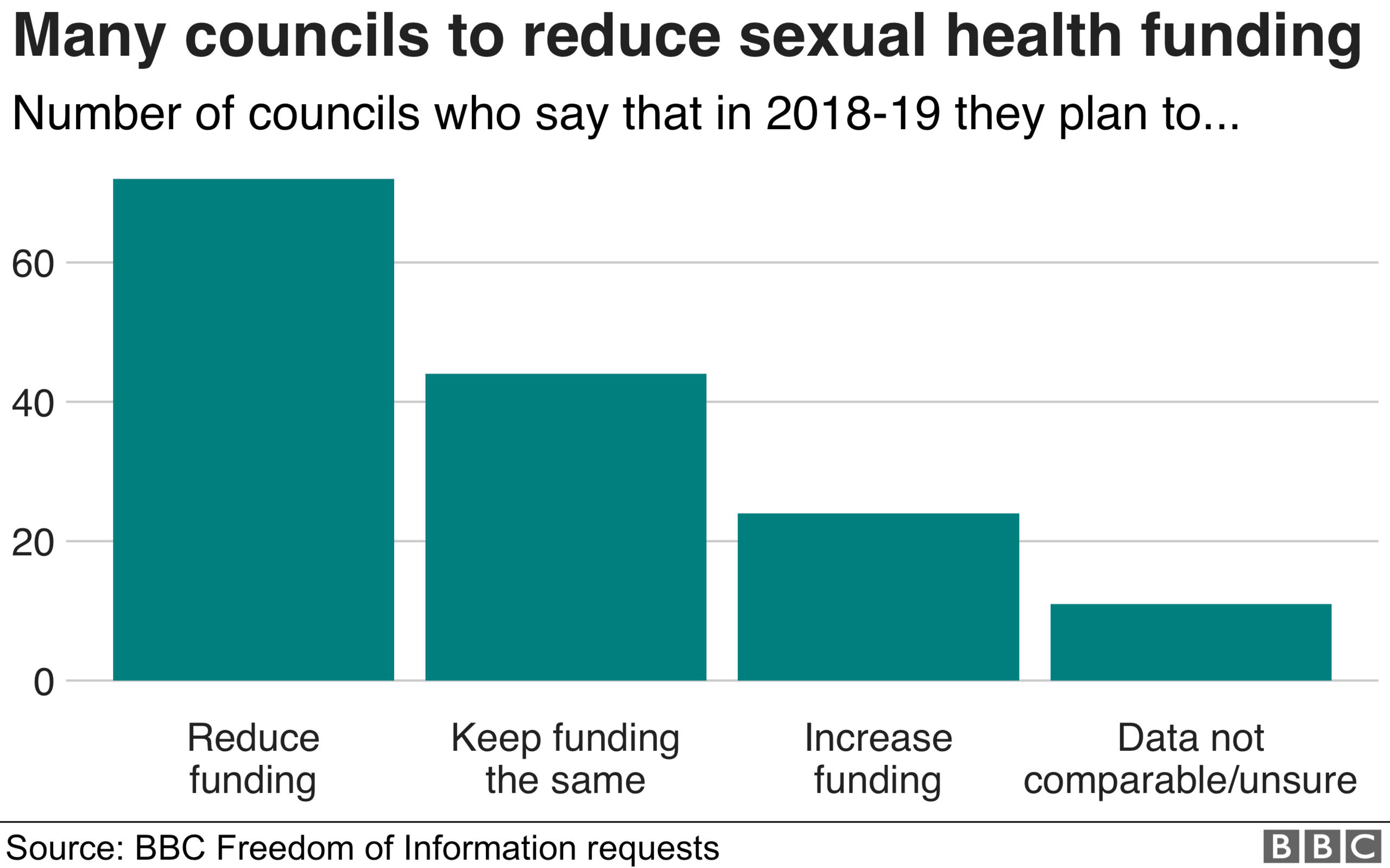
Some sexual-health clinics face closure or reduced hours as almost half the councils in England plan to cut spending, a BBC investigation reveals.
Of the 151 councils that responded to a BBC Freedom of Information request, 72 planned to cut sexual-health funding in 2018-19 compared with 2017-18.
Most said any savings would be made through efficiencies, but 16 councils said services would be cut or reduced.
The government said councils were being given money to spend on services.
Rationing
The BBC's FoI request reveals:
Some clinics in Suffolk, Cambridgeshire, Nottingham, Brighton and Hove, Doncaster and Norfolk are either facing closure or having to reduce their opening hours
People living in rural Suffolk have to travel further to access services following the closure of three clinics in April
Opening days for adult sexual-health services in Doncaster are being reduced from six to five a week
Cheshire East council plans to "restrict" free access to emergency contraception in pharmacies to women under the age of 25 because of the need to make "savings"
A popular clinic for students operating out of the Cripps Health Centre, on Nottingham University campus, lost its funding in March
"While we appreciate the value that discretionary services such as Cripps add to patient choice and access, during times of severe cuts to our operating budgets we cannot continue to provide those which are additional and complementary to core provision," Nottingham city council told the BBC.
Some councils, however, said they had managed to save money and improve services.
Waltham Forest, for example, said it would improve access by having more clinics and longer opening times, despite a drop in its budget.
Many areas are increasing the availability of home self-test kits, which can be ordered online.
And in London and Manchester "chem-sex" support groups have been set up to help those who use drugs as part of sexual activity.
Drug use in a sexual context increases the risk of transmission of HIV, hepatitis and other sexually transmitted infections, Public Health England has said.
Patients 'turned away'
Dr Anatole Menon-Johansson is clinical lead for sexual health at Guy's and St Thomas', in south London, as well as the clinical director for the charity Brook. His trust serves areas with some of the highest rates of sexually transmitted infections in the country, but reduced its clinics from six to three last year.
He said: "There is unmet need. STI rates are still very high. And we have clinics that are closing. The reality is it's not going to help.
"Last week, we turned away around 300 patients. However, this was around half the amount of patients we were turning away each week last year due to the measures we have put in place"
Dr Menon-Johansson said he had recently spoken to a patient who had gone to St George's hospital seeking help only to find the clinic there had been closed.
"He then went to the Vauxhall clinic and that had been closed. Then I saw him at the Walworth Road clinic, where it was third time lucky for him."
Harder to get an appointment
Having previously been diagnosed with genital warts, Liv Grosvenor, 24, from the North Norfolk coast, has regular check-ups, but her nearest sexual health clinic is now 25 miles away and an hour's drive.
It had moved to this less convenient location in 2015, Ms Grosvenor said, making it harder to reach by public transport.
"Since it's been moved and the funding's been cut, it's really difficult to access," she said.
Dr Olwen Williams, of the British Association for Sexual Health, said the FoI findings should "raise alarm bells".
"With the recent emergence of multi-drug resistant gonorrhoea and record levels of syphilis being detected, clinics are being closed at the worst possible time," she said.
The Royal College of Nursing also warned of a potential public health risk.
It said: "If people are not able to access services, then serious conditions go undiagnosed, untreated and spread further."
A government official said it had a "strong track record" on sexual health, with teenage pregnancies at an all-time low.
More than £16bn will have been given to councils to spend on public health over the five years from 2015 to 2020.
Responsibility for sexual health was taken away from NHS England and handed to councils in 2013.
Since then, STI testing and most contraceptive services have been overseen by local authorities.
In Scotland, Wales and Northern Ireland public health services are still run by the NHS.
Izzie Seccombe from the Local Government Association said: "It's good news that we've got growing demand because that means that young people are taking their sexual health really seriously, and being responsible. But it is difficult for us to match growing demand with a reducing budget."
- Published3 August 2017
