Radical Parkinson's treatment tested in patients
- Published

The drug is delivered via a "port" in the side of the head
A radical Parkinson's treatment that delivers a drug directly to the brain has been tested in people.
Patients in the trial were either given the drug, which is administered via a "port" in the side of the head, or a dummy treatment (placebo).
Both groups showed improved symptoms, meaning it was not clear if the drug was responsible for the benefits.
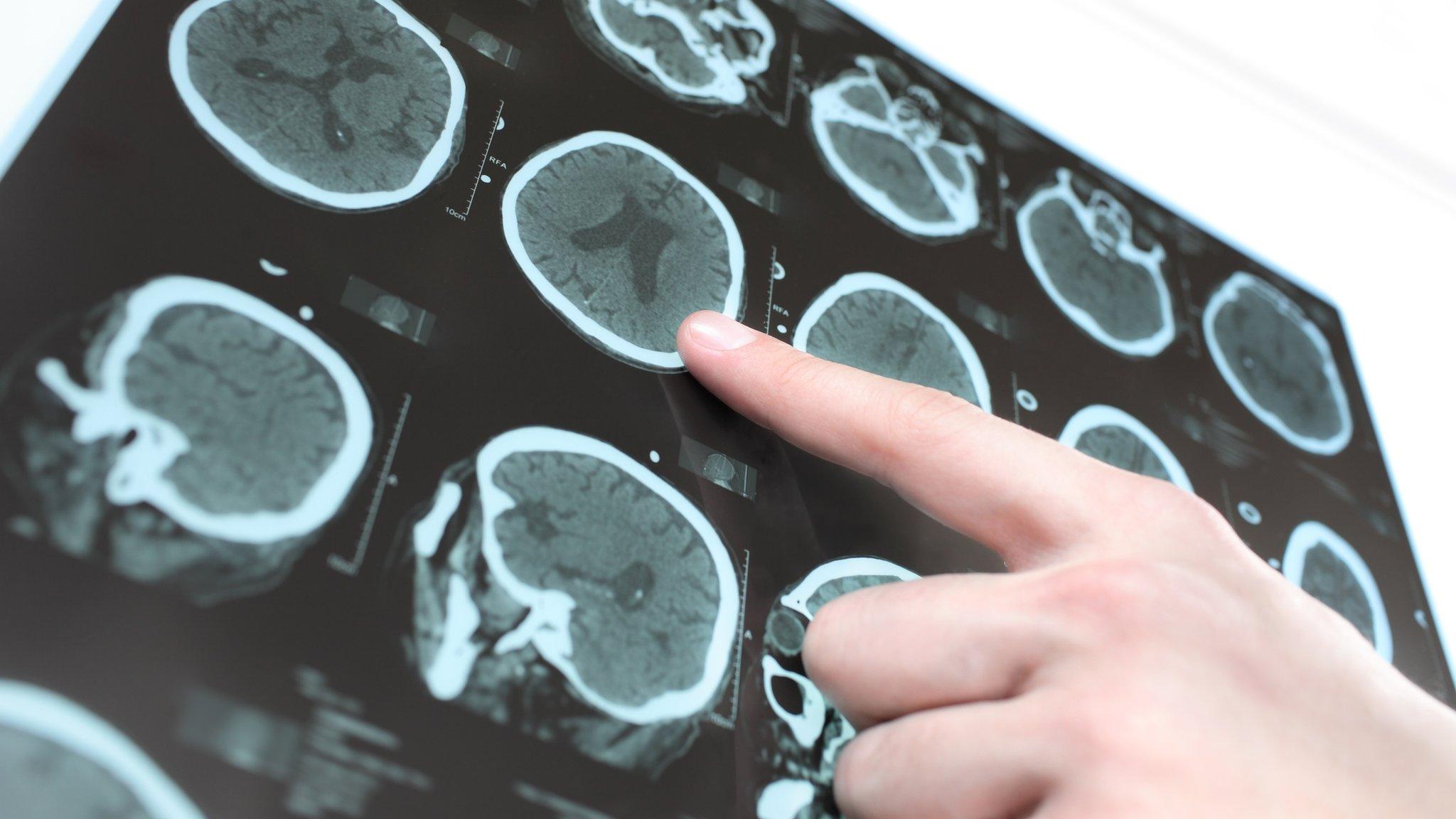
However, scans did find visual evidence of improvements to affected areas of the brain in those given the drug.
The study's authors say it hints at the possibility of "reawakening" brain cells damaged by the condition.
Other experts, though, say it is too early to know whether this finding might result in improvements in Parkinson's symptoms.
Researchers believe the port implant could also be used to administer chemotherapy to those with brain tumours or to test new drugs for Alzheimer's and stroke patients.
Parkinson's causes parts of the brain to become progressively damaged, resulting in a range of symptoms, such as involuntary shaking and stiff, inflexible muscles.
About 145,000 people in the UK have been diagnosed with the degenerative condition, which cannot be slowed down or reversed.
For this new study, scientists gave patients an experimental treatment called glial cell line-derived neurotrophic factor (GDNF), in the hope it could regenerate dying brain cells and even reverse the condition.
Participants underwent robot-assisted surgery to have four tubes placed into their brains, which allowed GDNF to be infused directly to the affected areas with pinpoint accuracy, via a port in their head.
After an initial safety study of six people, 35 patients took part in a nine-month "blinded" trial, where half were randomly assigned to receive monthly infusions of GDNF and the other half dummy infusions.
Dr Alan Whone, principal investigator, said patients in the trial had, on average, been diagnosed eight years previously, but brain scans of those given the drug showed images that would be expected just two years after diagnosis.
He said: "We've shown with the Pet [positron emission tomography] scans that, having arrived, the drug then engages with its target, dopamine nerve endings, and appears to help damaged cells regenerate or have a biological response."

'I feel it brought me time'
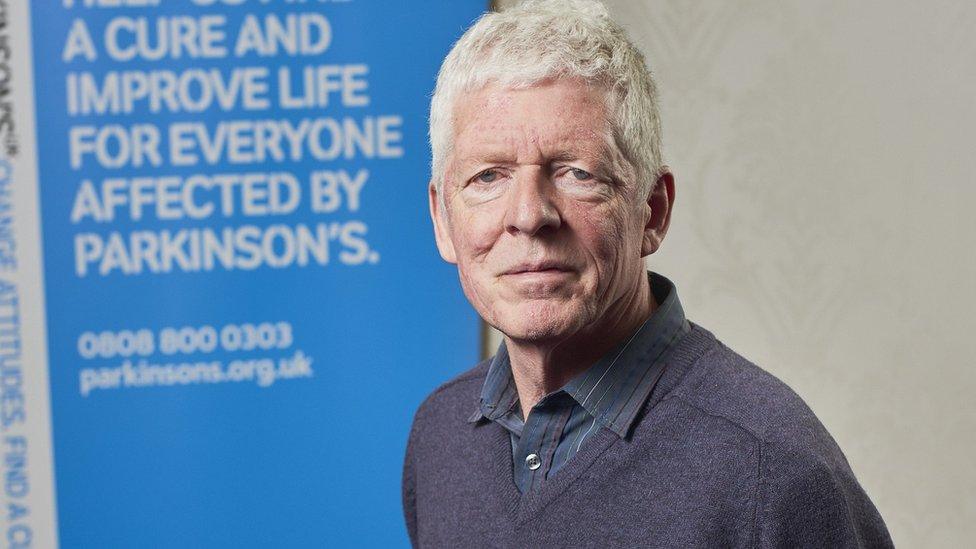
Tom Phipps, 63, from Bristol, said he had noticed an improvement during the trial and had been able to reduce the drugs he takes for his condition.
Since it ended, he has slowly increased his medication but is continuing to ride his bike, dig his allotment and chair his local branch of Parkinson's UK.
"My outcome was as positive as I could have wished for," he said.
"I feel the trial brought me some time and has delayed the progress of my condition.
"The best part was absolutely being part of a group of people who've got a similar goal - not only the team of consultants and nurses but also the participants.
"You can't have expectations - you can only have hope."

Following the initial nine months on GDNF or placebo, all participants had the opportunity to receive GDNF for a further nine months.
By 18 months, when all participants had received GDNF, both groups showed moderate to large improvements in symptoms compared with their scores before they started the study.
But the authors say the results need to be treated with caution because of the possibility of the placebo effect - when a patient feels better despite taking a medicine with no active ingredient.
Researchers hope that further trials could look at increasing the doses of GDNF or the duration of treatment.
'Great interest'
Experts said it was "disappointing" that the difference in symptoms was not significant.
But they said the study was still of "great interest" and warranted follow up research.
The findings from the trials are published in the medical journals Brain, external and the Journal of Parkinson's Disease, external.
The study also features in a two-part BBC Two documentary series, The Parkinson's Drug Trial: A Miracle Cure? on 28 February and 7 March, at 21:00.
- Published31 October 2018
- Published4 August 2017
- Published11 April 2018
