Opioid painkillers 'must carry prominent warnings'
- Published
Warnings are "tip of the iceberg", says addiction counsellor Nicki Hari
All opioid medicines in the UK will carry prominent warnings on their labels saying they can cause addiction, the health secretary has announced.
Matt Hancock acted after figures in England and Wales revealed a-more-than 60% increase in prescriptions for opioid painkillers in the last decade.
People needed protection "from the darker side to painkillers," he said.
Health experts welcomed the move, saying opioids can cause "life-altering and sometimes fatal addictions".
Opioids, such as morphine or fentanyl, can be highly effective for managing severe pain but they can also be highly addictive, the Department of Health (DoH) said.
It warned the number of prescriptions in England and Wales issued for these sorts of medicines had risen dramatically from more than 14 million in 2008 to 23 million last year.
The DoH added there are also some opioids available over the counter, such as codeine-based painkillers, which are weaker in strength but can also cause addiction.
From 2008 to 2018, the number of codeine-related deaths in England and Wales has more than doubled to more than 150, it said.
In Scotland, codeine-related deaths spiked at 43 in 2016, dropping to 27 in 2017, National Records of Scotland, external said.
In Northern Ireland, there were 16 codeine-related deaths in 2017, external.

What are opioids?
A large group of drugs used mainly to treat pain
Includes naturally occurring chemicals like morphine and codeine, as well as synthetic drugs
Codeine, morphine and methadone are among opioids judged by the World Health Organization as essential for treatment of pain and end-of-life care
Some opioid medications - methadone and buprenorphine - are used to help people break their addictions to stronger opioids like heroin
What are they used for?
Moderate and severe pain relief
Limited time treatment of pain that does not respond to standard painkillers like aspirin, ibuprofen and paracetamol
Usually used for acute pain - such as after surgery or terminally-ill cancer patients
Why are they dangerous?
They can be highly addictive
Pleasurable feeling that results from taking opioids can contribute to psychological dependence on the drugs
Higher doses can slow breathing and heart rate, which can lead to death
Mixing with alcohol or other sedatives such as benzodiazepines can also have serious consequences

Mr Hancock said: "I have been incredibly concerned by the recent increase in people addicted to opioid drugs.
"Painkillers were a major breakthrough in modern medicine and are hugely important to help people manage pain alongside their busy lives but they must be treated with caution.
"We know that too much of any painkiller can damage your health, and some opioids are highly addictive and can ruin lives like an illegal drug.
"Things are not as bad here as in America, but we must act now to protect people from the darker side to painkillers."

'Like thousands of insects inside your skin'

Lisa Peake, from London
I was prescribed painkillers for chronic neck pain after an accident in February 2014 but the pain didn't go away.
I was taking codeine four to five times a day, tramadol as a top-up once a day, as well as naproxen and co-dydramol four or five times a day.
Opioids affect your mental capacity, you feel dizzy, you can't concentrate and it's hard for you to do your job.
I went on a three-week hospital pain management programme in October 2016 and they helped wean me off the meds and rely on other methods of pain control.
I had all the symptoms, albeit to a lesser extent, of a drug addict doing the same.
It feels like you've got thousands of insects inside your skin. You can't find any comfort, you can't sleep and your bowel movements are shot to pieces.

Professor Dame Sally Davies, the chief medical officer for England, has welcomed the government action.
She said: "We know that long-term use of painkillers can lead to life-altering and sometimes fatal addictions, so I am delighted to see measures put in place to raise awareness of the risks of codeine and prescribed drugs.
"It is vital that anyone who is prescribed strong painkillers takes them only as long as they are suffering from serious pain.
"As soon as the pain starts to alleviate, the drugs have done their job, and it is important to switch to over-the-counter medication like paracetamol which do not carry the same risk of addiction that comes with long term use."

Analysis by Fergus Walsh, BBC medical correspondent
Until the late 90s in the UK, opioids were usually restricted to cancer patients and for those in acute pain following surgery, but then they began being increasingly prescribed for chronic pain.
As our population ages, the number of people living with low back or nerve pain is soaring. Opioids can be effective in the short term, but don't work for pain that lasts for months or years.
The medicine packets already contain leaflets warning about potentially dangerous side-effects and the risks of addiction. Making these more prominent may encourage patients and their doctors to discuss alternatives such as physical and talking therapies.
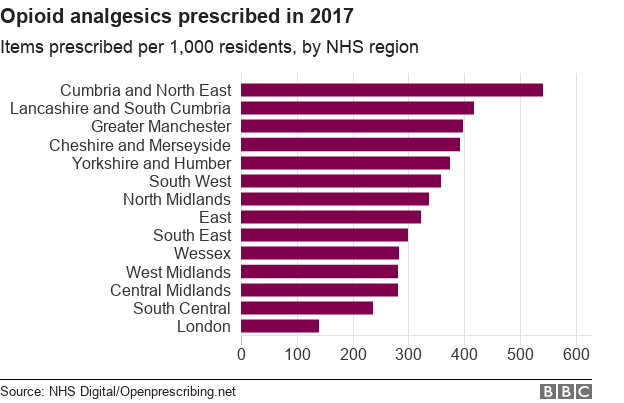
The variation in prescribing rates between NHS regions shows that it is possible to limit their use.
Things have been getting worse here, but are nowhere near as bad as the US which has four times the rate of opioid prescriptions as the UK.

Public Health England is already undertaking a review, external into prescription medication addiction and is due to report its findings this year.
Under Mr Hancock's plan, the Medicines and Healthcare products Regulatory Agency (MHRA) will have the power to enforce warnings on opioids packaging, following recommendations from the UK's Commission on Human Medicines (CHM) Opioid expert working group.
Dr June Raine, director of the MHRA's vigilance and risk management of medicines division, said: "This is an important first step to help minimise the risks of addiction associated with opioid medicines, while supporting patients to get the right information at the right time to support their care."
- Published22 July 2018

- Published19 March 2018

- Published15 March 2018

- Published25 October 2017