11 charts on the problems facing the NHS
- Published

The NHS faces a number of challenges and often tops the list of concerns voiced by the public, but what state is it actually in?
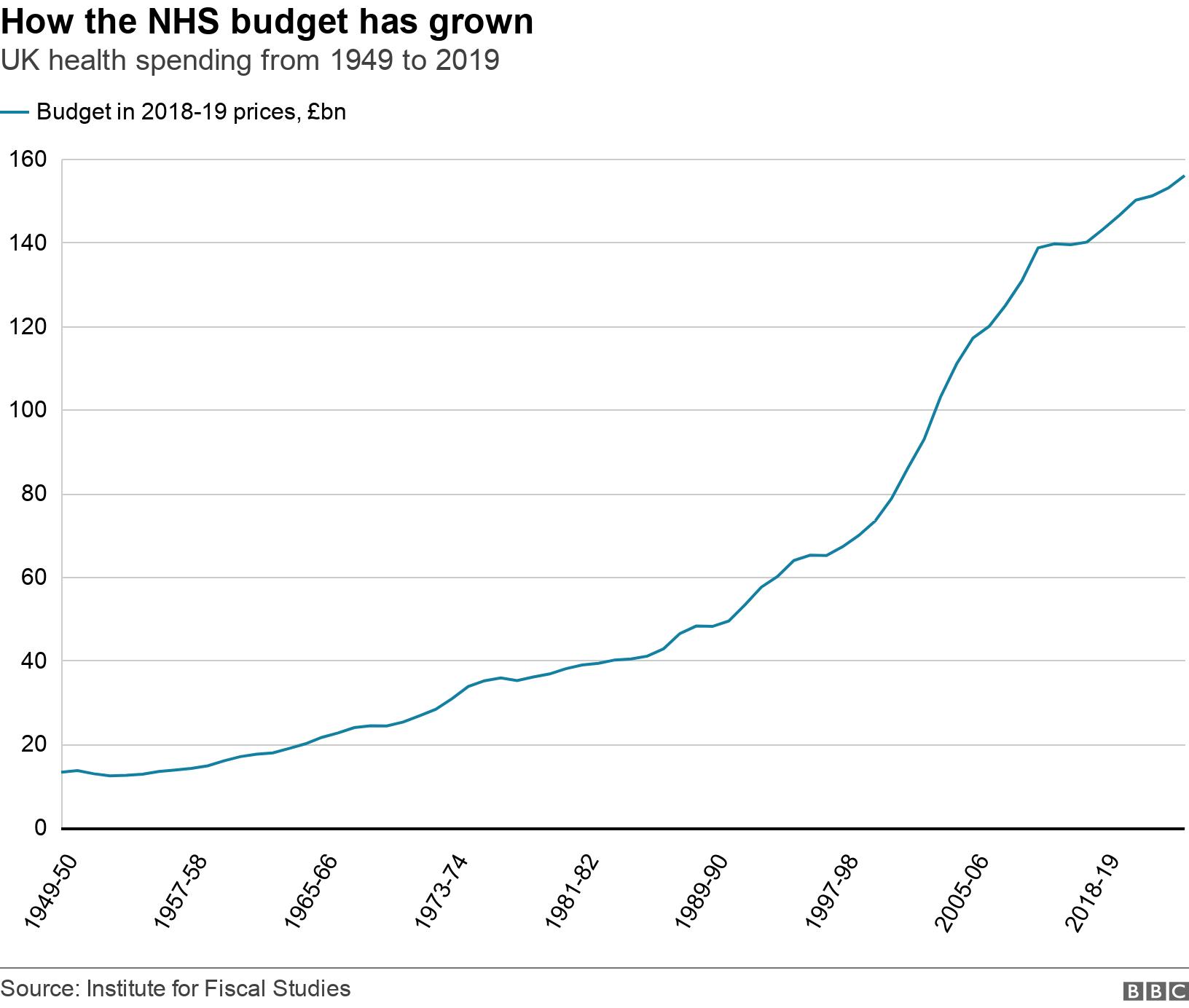
1. We spend more on the NHS than ever before...
Last year more than £156bn was spent on health across the UK - about 12 times the figure that was spent 70 years ago.
And that's after you adjust it for inflation.
It means today about 30p out of every £1 spent on public services goes on health.
2. ...but spending has slowed
Ever since the early 1950s the budget has been increasing, but the scale of those rises has varied quite considerably.
The average rise has been just over 4%. The biggest rises were seen under the Labour governments between 1997 and 2010 when the average annual rise was about 6%.
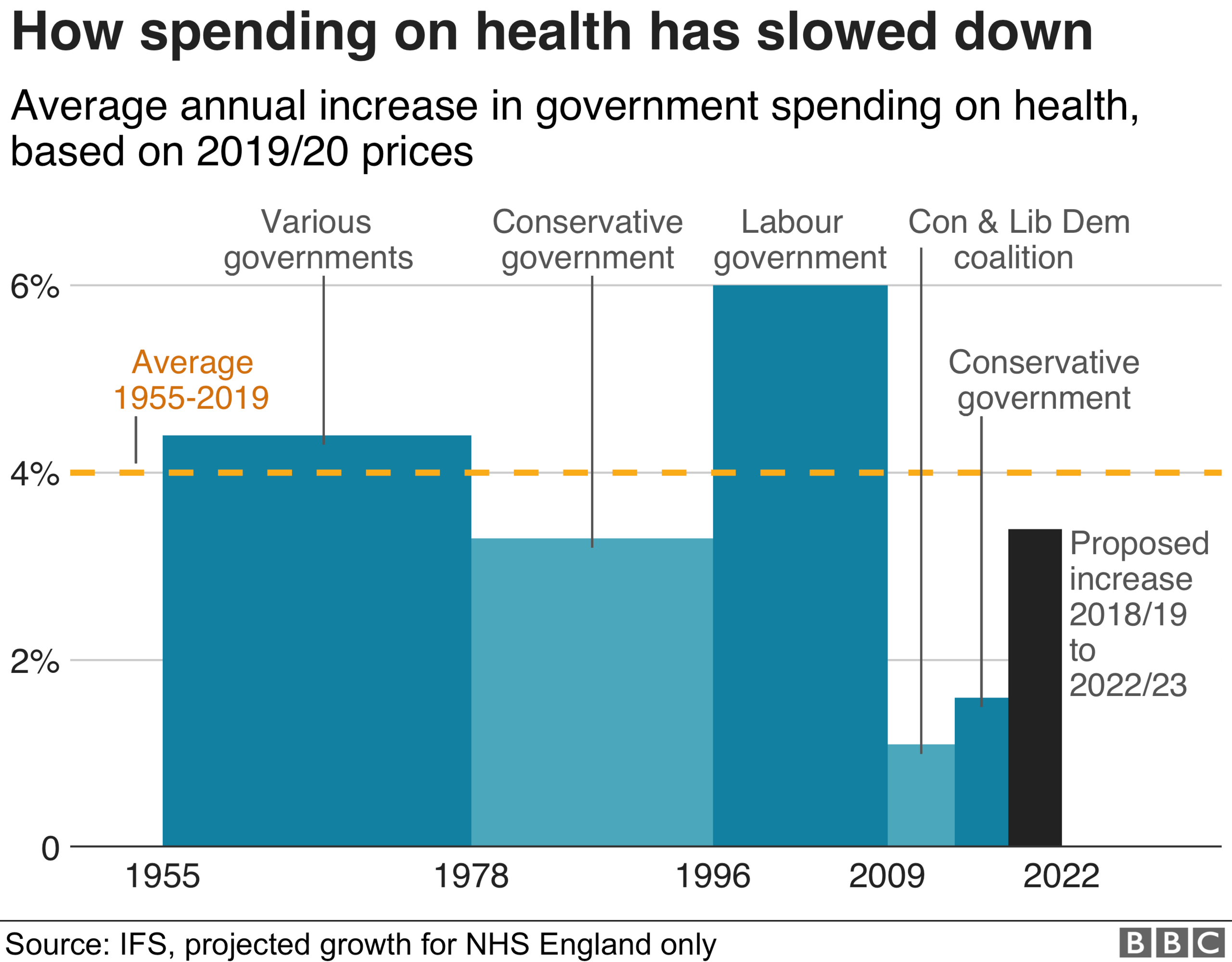
This dropped to 1% under the post-financial crisis coalition government between 2010 and 2015 - a figure which then rose under the majority Conservative government of recent years.
The Conservatives have said their five-year funding plan for the NHS will see the budget rise by an average of 3.4% a year above inflation. It means that by 2023-24 there would be £149bn of funding available.
By comparison, during the 2019 General Election, Labour proposed increasing it by 3.9% - bringing the budget to £155bn by 2023-24. The Lib Dems were marginally behind this coming in at £154bn.
3. Use of private companies has increased
Labour often talk about the risk of privatisation of the NHS, accusing the Conservatives of wanting to do a deal with US President Donald Trump.
Private firms are already involved in providing NHS care. Just over 7% of the budget goes on private providers, up from just over 5% in 2011-12.
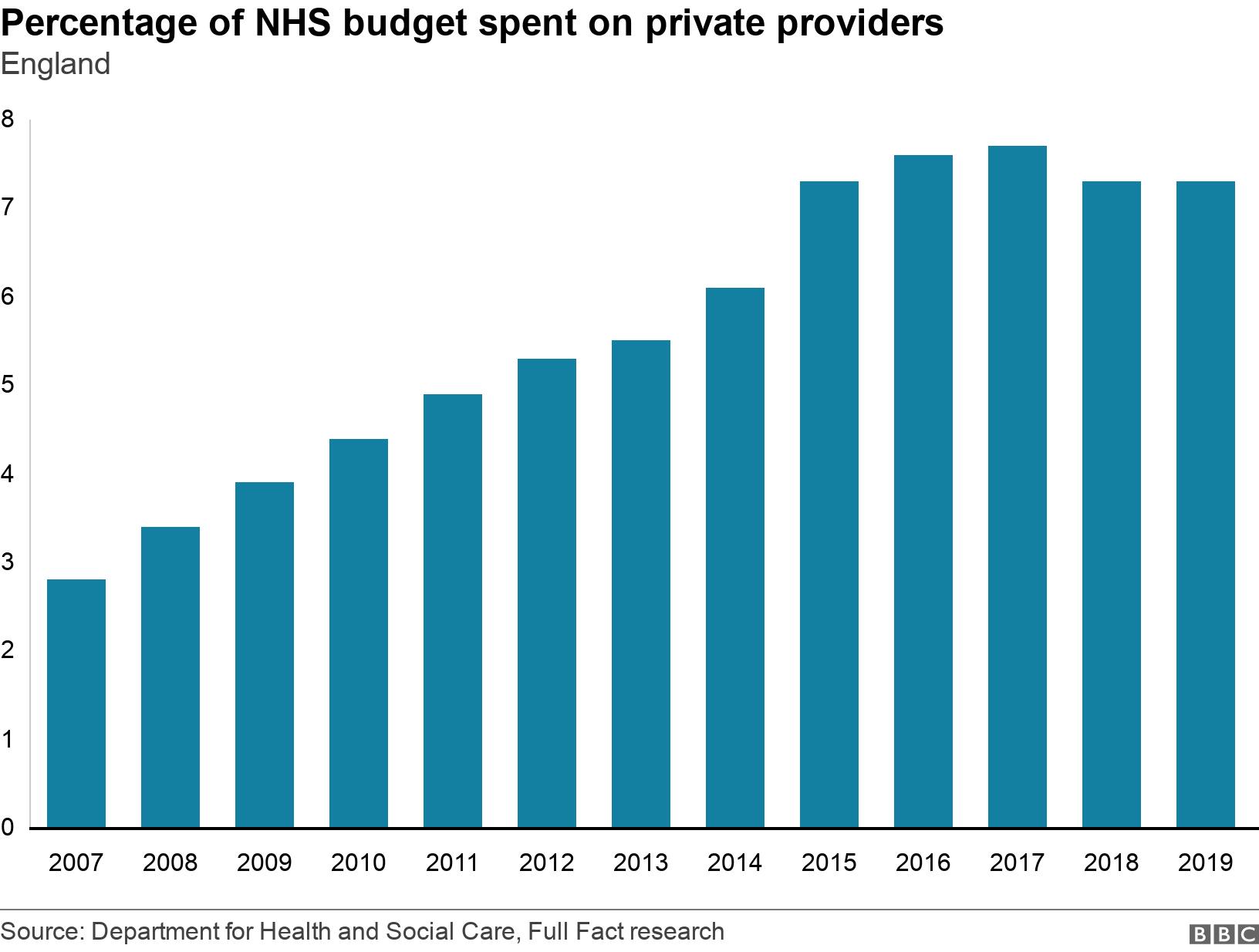
These can be deals to run a specific service or to take on some NHS patients for routine treatments like hip and knee replacements.
But it still leaves the overwhelming majority of care provided by the state and state-employed staff.
Actually, GPs are technically independent small businesses contracted to provide a service to the NHS - but they tend not to be considered as private providers.
NHS money also goes to the private sector to purchase drugs and equipment.
Nearly all of this is bought centrally so the NHS can use its bargaining power to negotiate good deals. A recent example of this was the agreement reached with Vertex to fund its cystic fibrosis treatments.
The NHS got a significant saving on the price the drug manufacturer originally wanted. Fears have been raised that US firms would want the NHS to agree more lucrative deals - they get more money for their drugs in their own country. But given the cost to the NHS of such a concession many doubt this is likely.
4. Waiting times are getting worse
There are three key targets for hospitals: covering A&E, cancer care and routine operations, such as knee and hip replacements.
All parts of the UK have been struggling to hit them.
The way they are measured differs between the UK nations.
The A&E target is the most directly comparable - in that each nation expects 95% of patients to be treated or admitted in four hours.
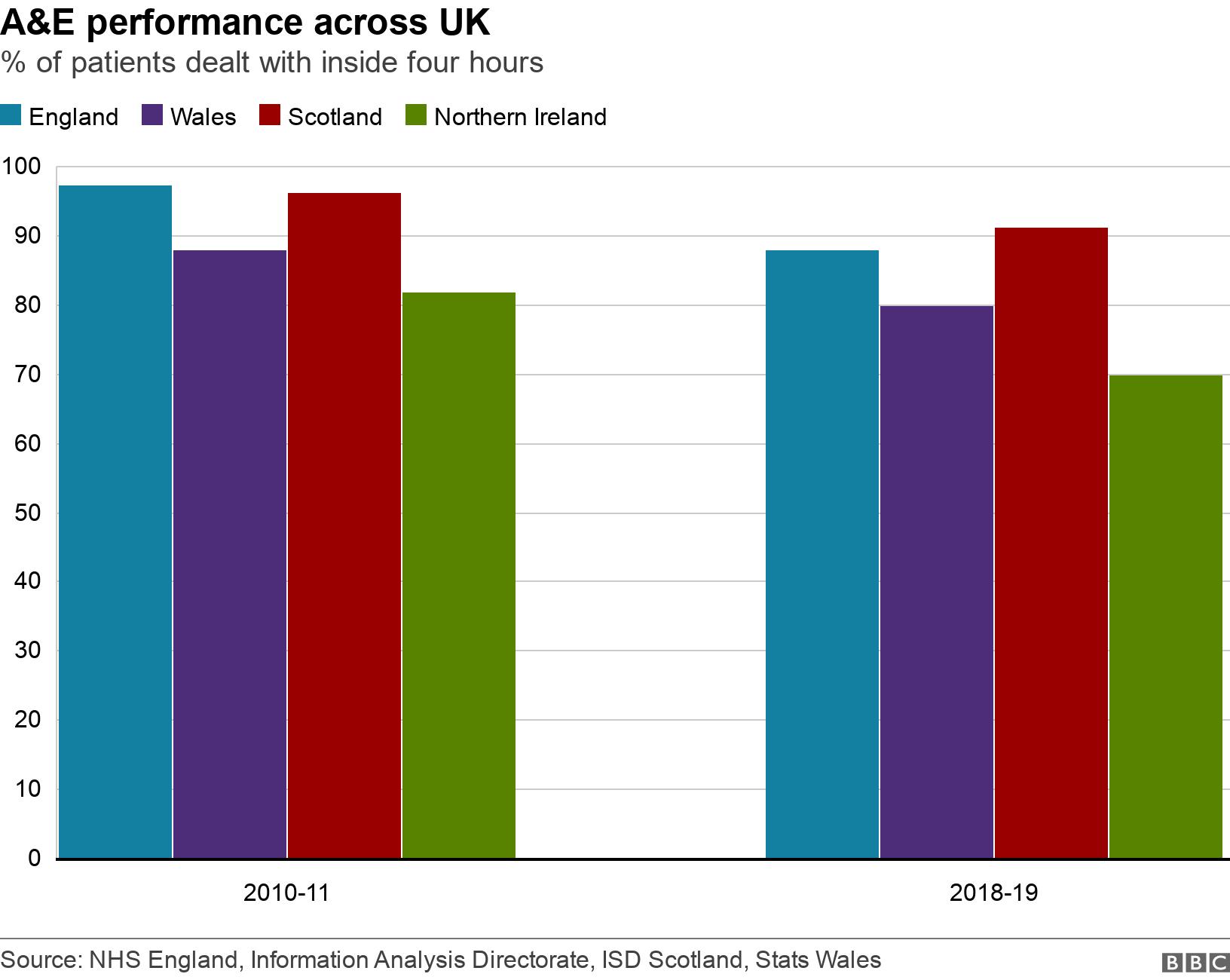
Performance is worse in Wales and Northern Ireland than it is in England and Scotland.
Scotland is the last nation to have hit the target - back in the summer of 2017.
Meanwhile, in cancer care patients are meant to start treatment within 62 days of an urgent GP referral. But that too is being missed, while waiting lists for routine treatments are rising.
In England it has topped 4.4 million - the highest on record. Some 15% have waited more than the target time of 18 weeks.
5. The population is ageing
The ageing population is certainly a major factor for the growing pressures - and it is one with which all health systems in the world are struggling.
Medical advances have meant that people are living longer. When the NHS was created, life expectancy was 13 years shorter than it is now.
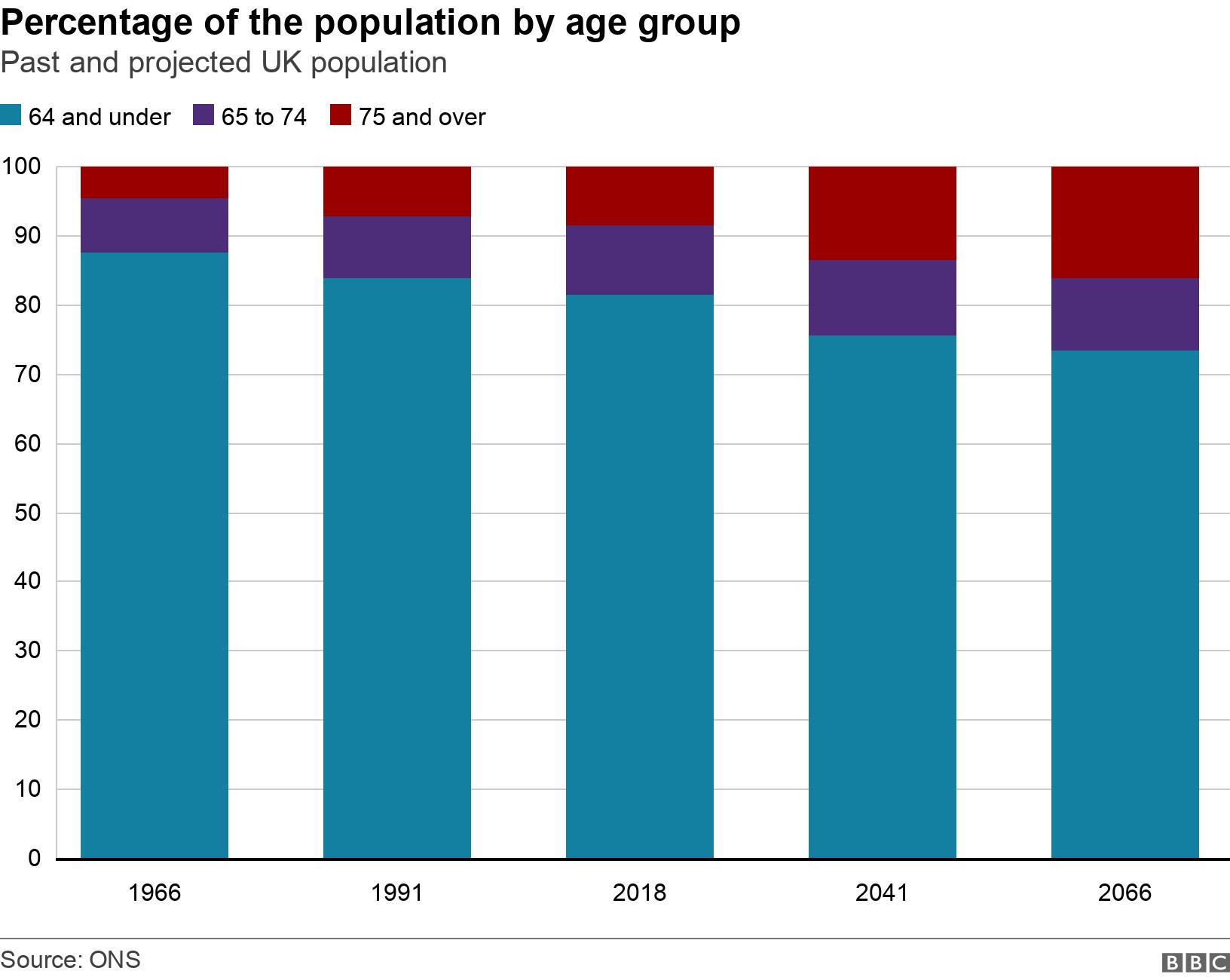
This is something to celebrate. Infectious diseases are no longer a significant threat. Heart attacks do not claim the lives of people early in the same numbers.
Even cancer is not the death sentence it once was - half of people now survive for a decade or more.
But this progress has come at a cost. People are living with a growing number of long-term chronic conditions - diabetes, heart disease and dementia. These are more about care than cure - what patients usually need is support.
6. Care for older people costs much more
That level of ill-health means the average 65-year-old costs the NHS 2.5 times more than the average 30-year-old.
A 90-year-old costs more than seven times as much.
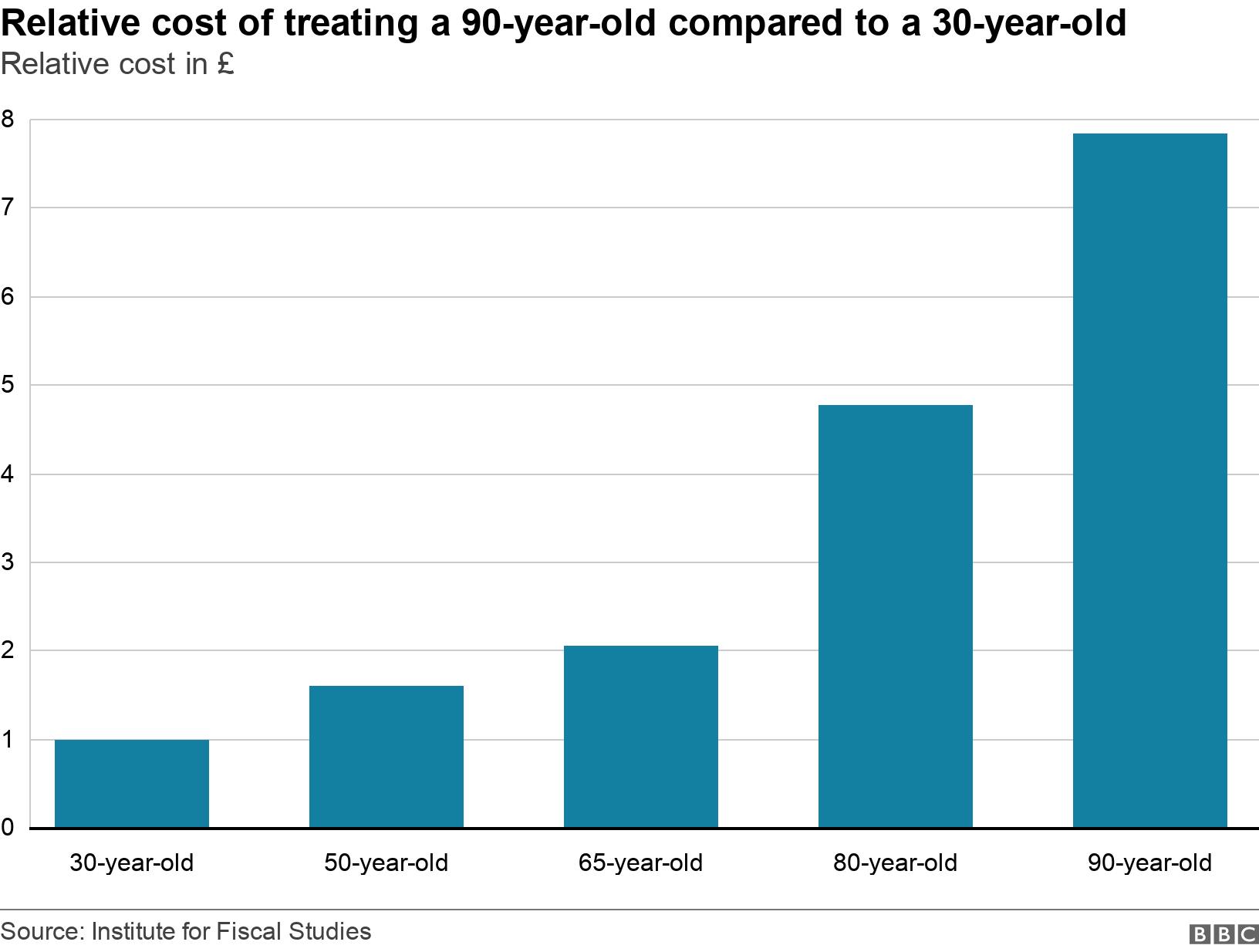
As the number of older people continues to rise so will the cost to the NHS.
This is compounded by other factors, including the rising cost of new drugs and high levels of obesity. A third of adults are so overweight they are risking their health significantly.
All this contributes to what health economists call health inflation - the idea that the cost of providing care outstrips the normal rise in the cost of living across the economy.
This is why health has tended to receive more generous rises than other areas of government spending.
7. The UK spends a lower proportion on health than some other EU countries
But despite this the UK has been left trailing some other parts of Europe when it comes to spending as a proportion of GDP, which is a measure of the size of the economy.
It is a gap that has widened since the previous Labour government was in power from 1997 to 2010.
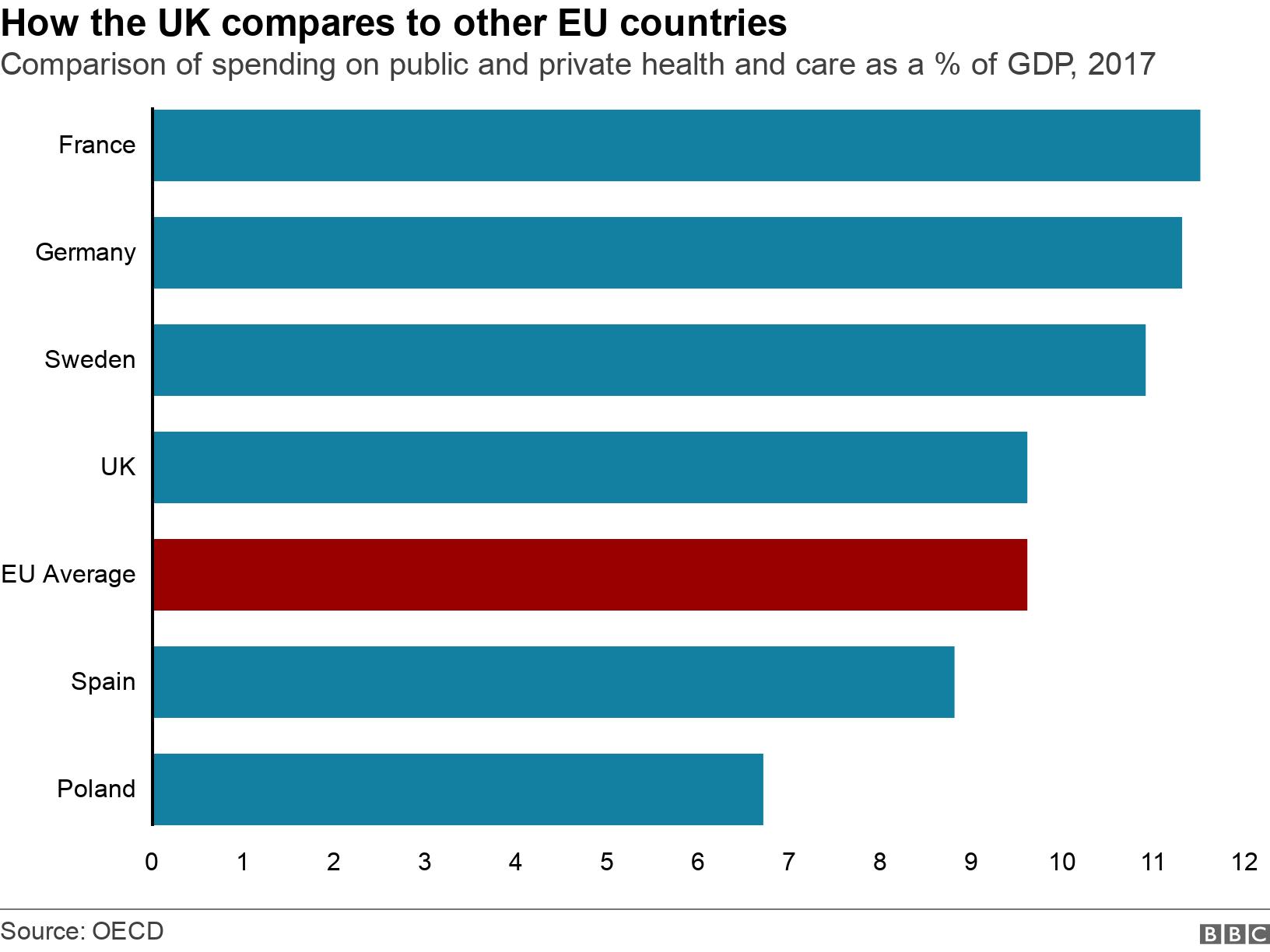
The result, as you would expect, is fewer beds, doctors and nurses per patient in the UK than the big spenders, which tend to tax people more.
Germany, for example, has almost twice as many nurses per capita, external than the UK.
8. The number of vacancies is high...
But the lack of staff in the NHS is not just because of less spending, the health service cannot even fill the posts for which it has got funding.
The NHS in England has nearly 100,000 jobs unfilled at the moment, external.
The total represents one in 12 of all the posts in the health service and would be enough to staff 10 large hospitals.
It includes about 40,000 nurse posts and nearly 10,000 doctor vacancies.
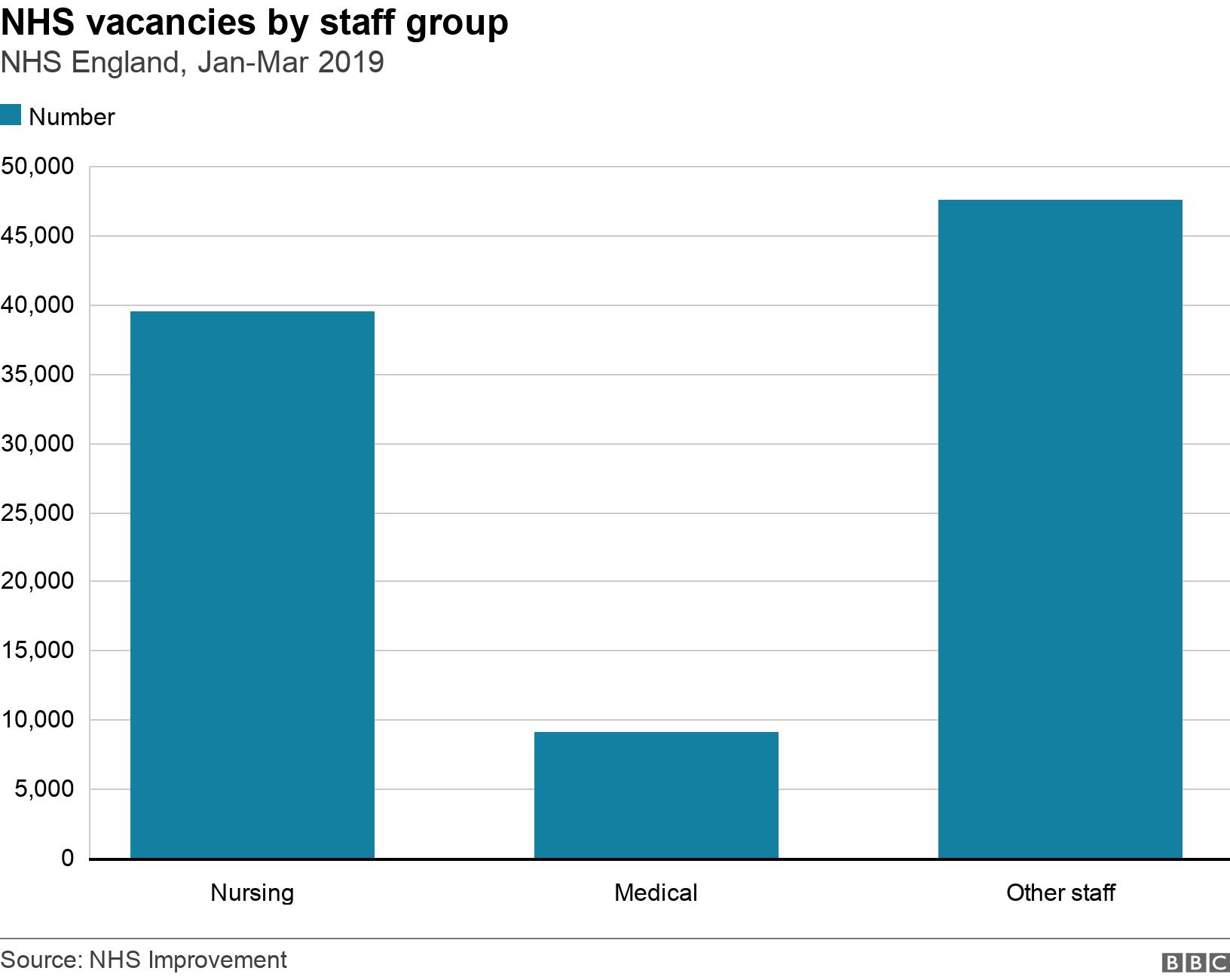
Some of the gaps are filled using overtime and agency staff, but some simply go unfilled.
There are various initiatives in place to recruit and retain staff.
And the number of training places for doctors and nurses are increasing.
9. ...and building works are falling behind
While the government has been able to put more money into the NHS, one element of the budget that has been cut is the money set aside for capital projects.
That covers the cost of infrastructure, such as building works and IT.
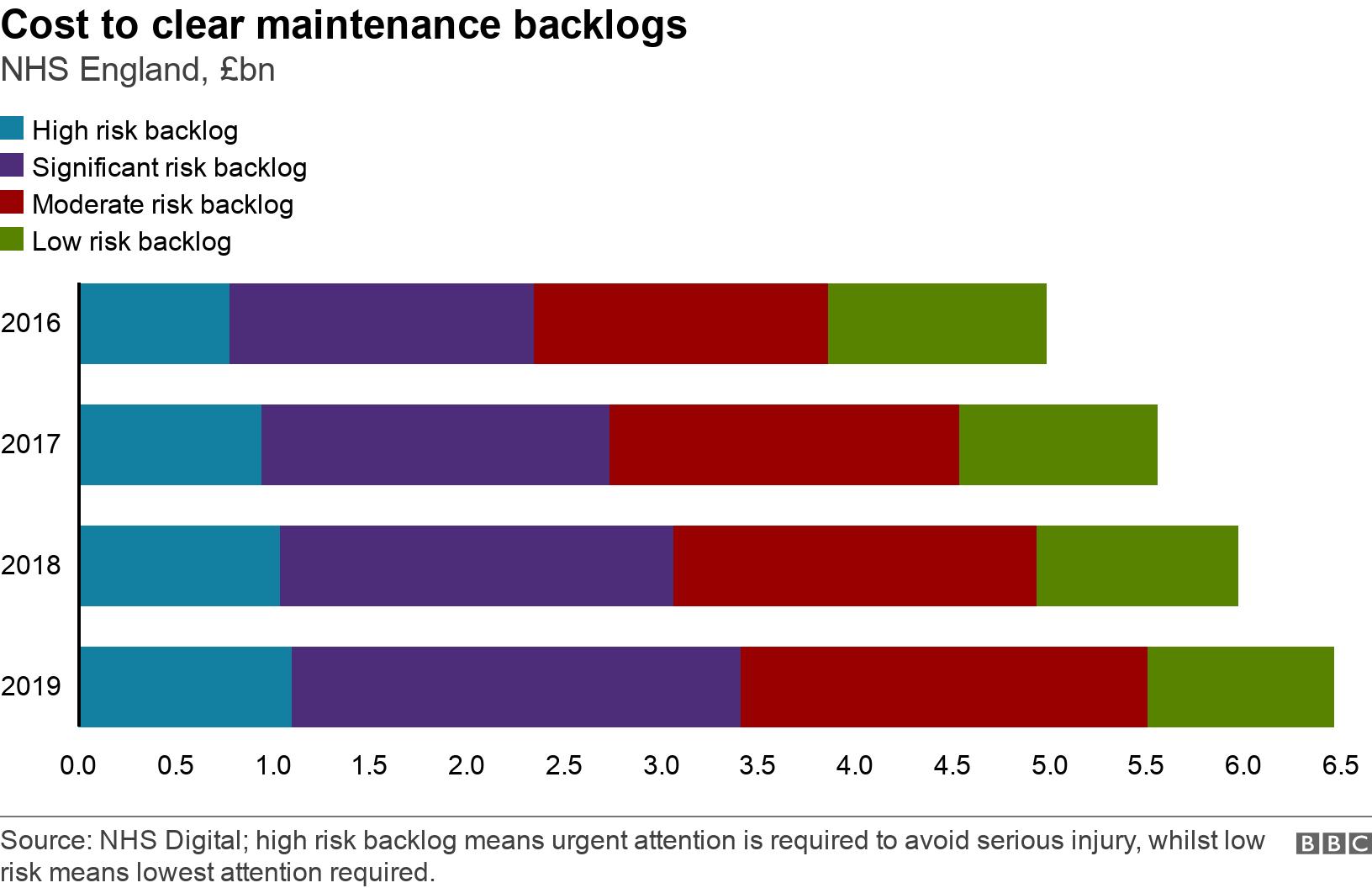
In recent years that has resulted in a growing maintenance backlog with hospitals having to contend with leaky roofs, out-of-date equipment and crumbling buildings.
The capital budget increased by £1bn for 2019-20, bringing the budget up to £7bn.
10. Not many older people get free care
The NHS is also under pressure because of the problems in the social care system.
Social care includes day centres, help in the home for tasks such as washing and dressing, and good quality care in care homes during the final years of life. It is seen as essential to keep people well and living independently - and out of hospital.
The system is means-tested in England, which means only the poorest receive help from councils towards the cost of care.
But even then it is heavily rationed. The result is growing numbers of older people going without care.
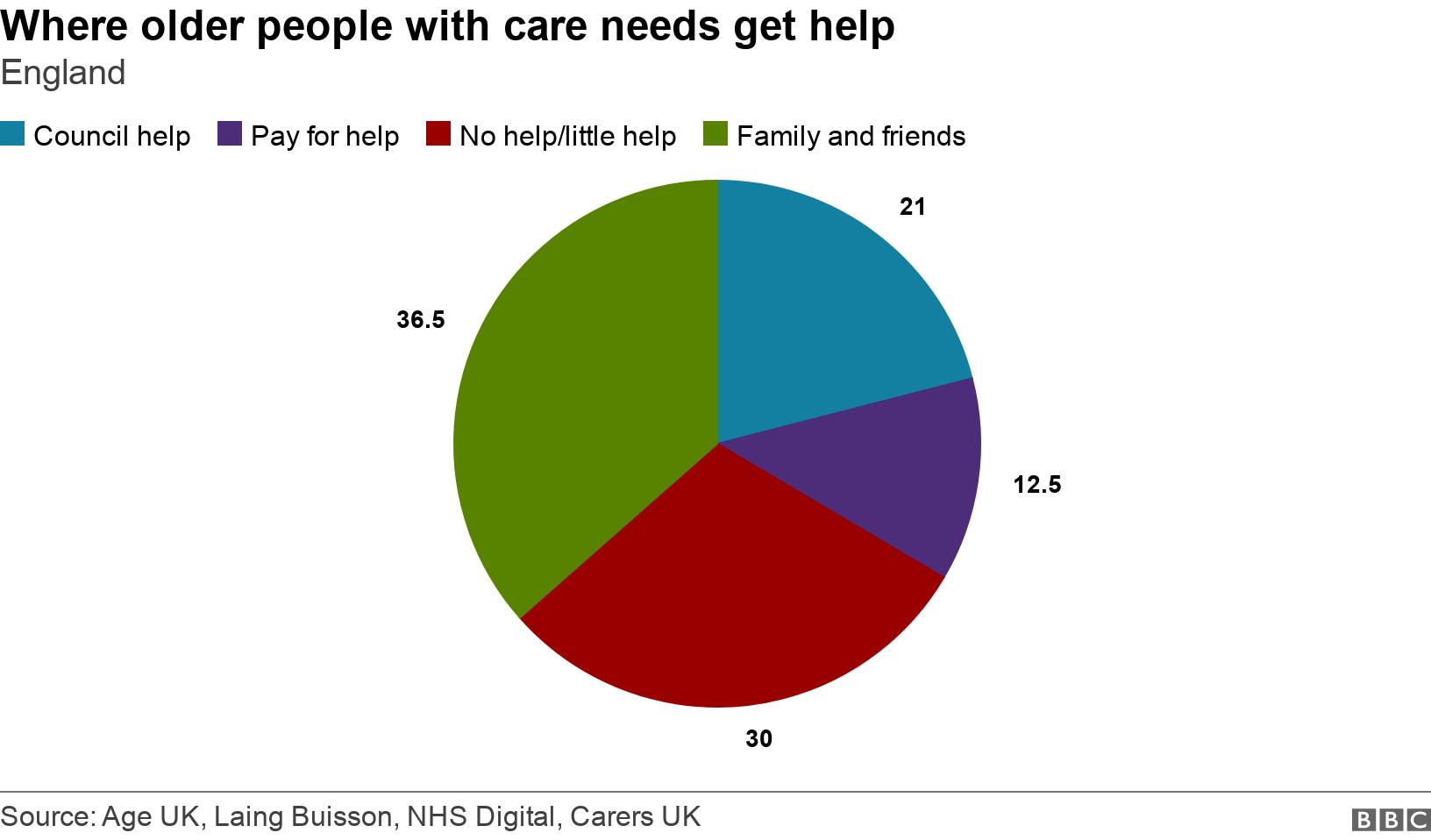
According to Age UK, 1.4 million people over the age of 65 are not getting the care they need.
That represents one in seven of all older people and is a rise of nearly a fifth in two years.
This lack of care in the community has been directly linked to the growing pressures on hospitals by the Care Quality Commission, the body responsible for regulating standards across health and social care.
The regulator believes that without reform of the system, the extra money being put into the NHS could be swallowed up without a noticeable improvement in performance.
The other parts of the UK can make a case for being more generous in this respect - home care is capped in Wales and free for the over-75s in Northern Ireland, while Scotland provides free personal care (washing and dressing) in both care homes and people's own homes.
11. Satisfaction remains high
Despite the challenges being faced by the NHS, the majority of the public say they are satisfied with services.
The British Social Attitudes poll of nearly 3,000 people found 53% of people in England, Scotland and Wales were satisfied with services in 2018.
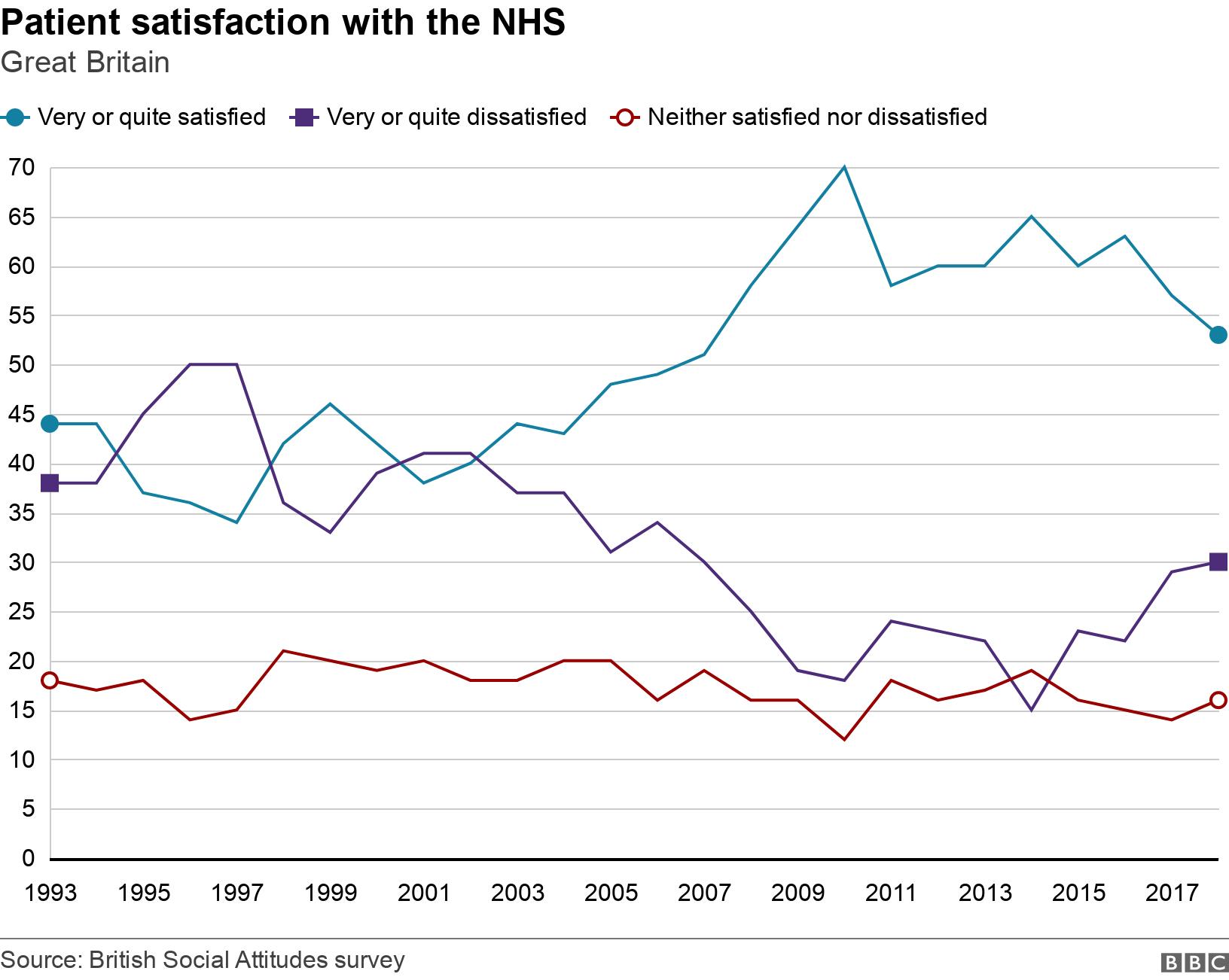
But levels of satisfaction are falling.
The latest score was a three percentage point drop since 2017 and the lowest level since 2007. A peak of 70% was seen in 2010.
Experts say waiting times and a lack of staff were major concerns as ratings for GPs dropped to an all-time low.
- Published30 October 2018
