Coronavirus doctor's diary: A super-spreading funeral that led to three deaths
- Published

Physical contact is one of the main ways the virus spreads
In March, before the lockdown began, the Hussain family held a big funeral in Bradford's Grand Mosque. Tragically, many mourners fell ill with Covid-19, including the dead man's son, Mohammed. But while three family members died, Mohammed eventually pulled through, writes Dr John Wright of the Bradford Royal Infirmary.
Being intubated and ventilated in intensive care turns out to be a long, rocky road. In Bradford, of the 49 Covid patients who have been admitted to our ICU so far, most have been placed on intubated ventilators. So far seven of these patients have come off ventilation.
Mohammed Hussain, a criminal lawyer from Bradford, was one of the first. He is one of our success stories.
The 51-year-old was unconscious for five weeks and was very disconcerted when he woke up in what looked like a science fiction film with everybody wearing visors and masks and gowns - he couldn't remember how he got there. He had entirely missed the month of April.
"I remember them asking me to go on the Recovery trial to try certain drugs and I said 'Yes.' But that's my last memory until I was waking up weeks later," Mohammed told me.

Mohammed Hussain in his hospital bed, making a video call to his son

While under sedation, he dreamed that his family had experienced a terrorist attack. And when he came round he remained uneasy.
"There was some paranoia to begin with. I thought, 'These people are trying to trick me. What's going on, what's all this about?'"
This kind of delirium is quite normal for patients who wake up from critical care, says ICU consultant Dr Debbie Horner, clinical director for the anaesthetics and intensive care department. "It's common for patients to feel very suspicious and anxious about what's going on around them. You can understand it, people are telling you that it's more than a month later and everyone's wearing really strange clothes."

Dr Debbie Horner says intensive care patients are often disoriented when they wake up
Usually it's possible to give people advance warning before they get intubated, but Mohammed deteriorated quickly. He fell ill in March, following the funeral of his father, Noor, who was in his 90s.
Noor Hussain had come over from Pakistan in the 1960s to work in the mills in Bradford. He raised his family here, but it was always his wish to be buried in Mirpur.
"He was an old soldier who fought in the Second World War, in Burma, and he was a very determined man. He wanted to be buried next to his brother in Pakistan and I honoured that wish for him," Mohammed told me.
Noor Hussain died on 10 March. The funeral gathering started that afternoon. It is a very large and respected family, so people travelled from across the UK - about 600 came to pay tribute at Bradford's Grand Mosque on the first day.
The following day Mohammed flew to Pakistan with his father's body - his mum and his wife went with him. But back in Bradford, the funeral continued for another two days. On Thursday 12 March, 500 mourners came and shared a meal.
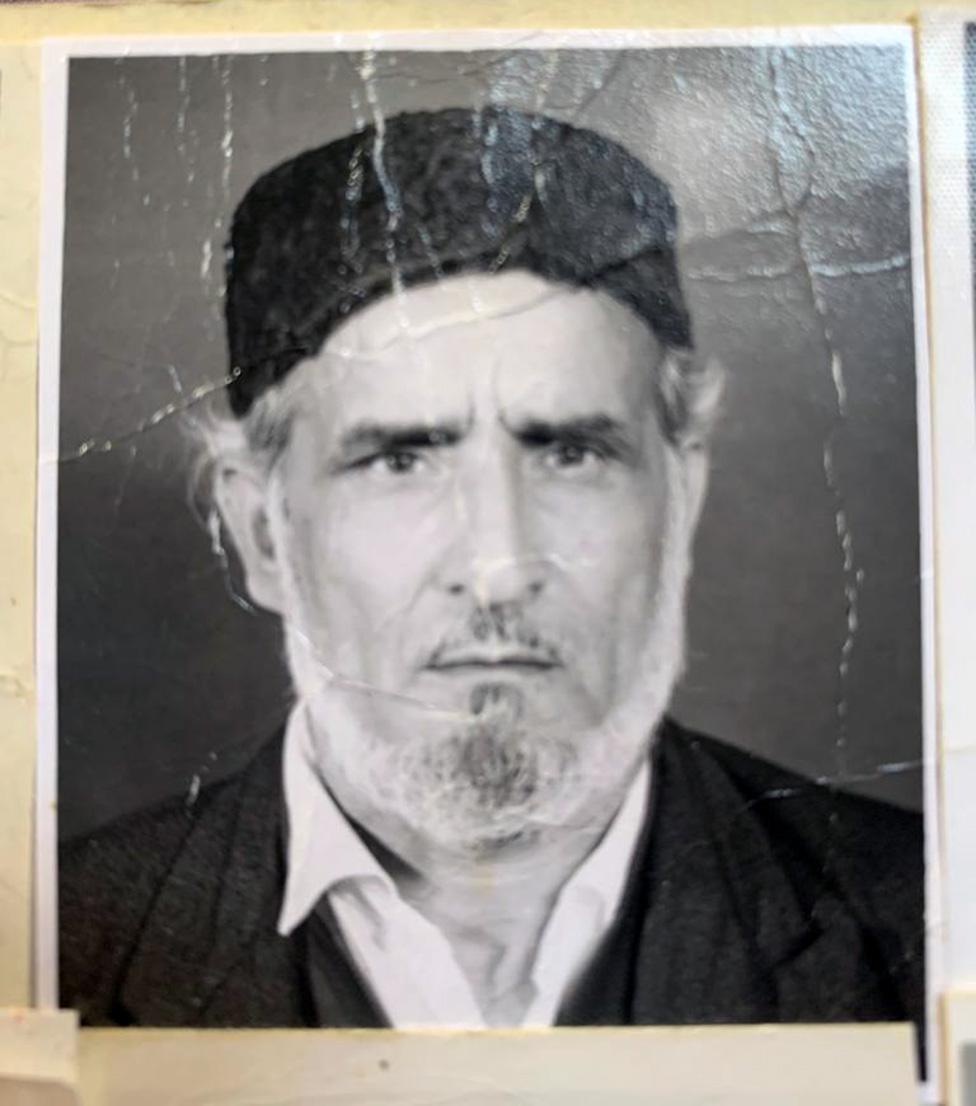
Noor Hussain when he was younger - his wish was to be buried in Pakistan

About a week later, people began to fall ill with Covid-19. The first was Mohammed's cousin's 24-year-old son - one of the first Covid patients in Bradford to be admitted to ICU. Three further members of that household also developed symptoms, one of them also going to hospital. And other relatives were hospitalised too, both in Bradford and Oldham.
It seems clear that someone at the funeral - possibly one of the mourners from Bradford, possibly one of the visitors from further afield - was infected with the coronavirus and that many people contracted it there.
"If you start looking at the number of cases that have come from that funeral, it's easy to see how quickly it spread," says Mohammed's son, Haroon, a radiologist.
"At the funeral you shake each other's hand and talk to people, you're very close.
"The country went into lockdown shortly after, and the reports are coming out now that coronavirus was in the population for a significant period of time before we realised. So if you've got a gathering of people, it increases the chances that maybe one of them has it."
Haroon can list eight family members who were hospitalised and three who died.
We have seen other patients who became ill after funerals and family gatherings in this same period, just before the lockdown. It's the close physical contact - hugging and shaking hands - that seems to create such a high rate of transmission. For the same reason, weddings and parties are also super-spreading events.
By the time Mohammed returned home from Pakistan on 18 March, Haroon and his brother, who live with their parents, had symptoms too.
"We tried to distance ourselves," says Haroon. "But when you're living in one household that's nigh-on impossible - there's only a certain number of bathrooms, there's only one fridge, one kitchen."
Mohammed was concerned about catching the virus because he is asthmatic, but that Saturday he developed symptoms. He stayed home for nine days, getting progressively worse, until his sons called 999.
"We walked him into the ambulance," says Haroon. "That was a very emotional moment as we couldn't go with him and we didn't know when we would see him again."
When Mohammed arrived at Bradford Royal Infirmary, he saw his uncle in the waiting room, also wearing an oxygen mask. Sadly, he has since died.

Front line diary

Prof John Wright, a doctor and epidemiologist, is head of the Bradford Institute for Health Research, and a veteran of cholera, HIV and Ebola epidemics in sub-Saharan Africa. He is writing this diary for BBC News and recording from the hospital wards for BBC Radio.
Listen to the next episode of The NHS Front Line on BBC Sounds or the BBC World Service
Or read the previous online diary entry: 'They say I have blood on my hands'

Mohammed was intubated and put on a ventilator. "During that time, people are deeply sedated and their muscles are paralysed with medicines to allow the oxygen to get into the body," says Debbie Horner.
Twice a day, Mohammed was proned, turned from front to back, to try and get as much oxygen into his body as possible by stimulating different bits of the lungs. This was done by a team of radiologists who volunteer to do this - they call themselves the Ratters - the Radiology Turning Team.

The Ratters - a team photo
At the start of this crisis, Covid-19 was thought to be primarily a lung disease where the life-saving treatment would be intubated ventilation, with patients sedated in intensive care. As the weeks have passed, clinicians have increasingly turned to less invasive ventilators called CPAP machines, which blow oxygen into the lungs, keeping them inflated - at Bradford we were using them from an early stage of the epidemic and putting patients on them at an earlier stage of their illness than some other hospitals.
Predictions in March were that 30% of patients would be on ventilators in intensive care units. As it's turned out, it's less than 20% nationally and less than 10% in Bradford, suggesting that this early and less invasive treatment is effective.
"I genuinely believe we've managed to pitch it right here," says Dr Tom Lawton, a consultant in critical care. "By using simple machines that are designed to make it all as easy as possible, and having brilliant staff that are prepared to jump in and do everything - even care that they're not used to delivering in that kind of environment - we haven't brought as many people to intensive care as we thought we would. And yet, our patients don't seem to have suffered as a result."
Preliminary data shows the death rate of Bradford Royal Infirmary is 23%, that's lower than national figures. However in ICU the death rate is 50%, in line with other ICU rates.

Mohammed's first taste of pineapple juice after ICU was "like a drink from heaven"
Once out of intensive care, Mohammed Hussain began a slow process of rehabilitation on a stroke ward.
His shoulder was damaged during proning and he needed additional physio - he couldn't move his right arm much and so it was difficult for him to feed himself.
He is full of gratitude. "Believe me, the people who work in ICU, in this crisis, putting themselves at risk, they are the most amazing people," he says.
"It's not just the medical treatment, but it's the human touch. It's the depth of the conversations, the genuine interest and how you develop relationships. It contributes massively towards you getting better.
"I remember when I was first taken upstairs on the ward, this poor doctor was running various tests and he went to get me a drink - he brought me pineapple juice. It was like a drink from heaven.
"Sometimes the enormity of what we've been through affects me and makes me emotional."

Haroon Hussain kept in touch with his father via video calls
During the five weeks that his dad was unconscious, Haroon kept everyone updated via Whatsapp.
"There were so many people worried about him," he says. "My dad is incredibly well-known in the community and the messages were going to hundreds of people throughout the world. Everywhere you go, you meet people who my dad has helped."
Looking through the replies from his hospital bed, Mohammed spotted a theme: "Oh, he's too stubborn, he's too tough, he'll be all right…"
"I didn't know that's how I was viewed by people," he says.
But Haroon isn't having it. "You did know that, that's a lie!"
Mohammed finally left hospital on Tuesday, to a standing ovation from ward staff.
I think one of one of the things that we didn't really do right at the start was celebrate those successes of patients leaving the ward - you tend to focus on the more tragic cases. So we have got better at that, and every patient that is discharged now, is a source of great joy.
Allow X content?
This article contains content provided by X. We ask for your permission before anything is loaded, as they may be using cookies and other technologies. You may want to read X’s cookie policy, external and privacy policy, external before accepting. To view this content choose ‘accept and continue’.

A couple of days ago Haroon updated us on what happened next.
"When I went to collect him from the hospital I didn't tell the rest of the family. I called them all down saying I needed to speak to them, and there was Dad sitting in his armchair. It was an amazing moment, just phenomenal, to have him home.
"He's just been out in the garden for the first time today and he was elated. He gets very tired very quickly so it's a slow process, but he's surrounded by love."
And Haroon's mum has now returned from Pakistan, so the family is together again. They're overjoyed.
Follow @docjohnwright, external and radio producer @SueM1tchell, external on Twitter
Correction 19th May 2020: An earlier version of this article wrongly included a picture of the Central Mosque Bradford in Westgate. This has been removed and the article amended to make clear that the funeral of Noor Hussain took place at the Bradford Grand Mosque.

Mohammed Hussain at home in his favourite chair

You may also be interested in:
Government advisers have been considering since March whether to include loss of smell among the criteria for deciding whether someone has Covid-19. Evidence that it is one of the symptoms is already strong and some scientists argue this is now an urgent step, as the lockdown is eased.
Why hasn't the UK listed loss of smell as a symptom of Covid-19?