Coronavirus doctor's diary: 'Our hospitals weren't made to use this much oxygen'
- Published

Shortages are dogging the fight against the coronavirus. At Bradford Royal Infirmary (BRI) it's still only possible to test six staff for the virus per day, consultants have been making their own personal protective equipment, and - as BRI's Dr John Wright reports - there's an urgent need to save oxygen.
6 April 2020
We are about a week away from the estimated peak of the epidemic. Our mainstay of treatment is to simply keep patients breathing, and two issues are preoccupying us - ventilators and oxygen.
It's become clear that the UK is pretty low down the international ventilator league table. Although we put in hasty orders for more, there appears to be a bit of a run on them, and we're worried that our order won't arrive in time to meet the Covid-19 peak.
However, there is growing evidence that a simple machine used by patients with sleep apnoea (snoring and interrupted breathing) in their own bedrooms can be an effective alternative. And Dr Tom Lawton, one of our ingenious intensive care consultants, has managed to get his hands on 100 of them from a local manufacturer.
Oxygen is the other priority.
The manufacturers are working around the clock to keep up with demand, but hospitals just aren't built to provide the flow of oxygen needed to keep so many patients on ventilators - and we're finding that our infectious "red zone" wards can only take a maximum of 10 ventilated patients before the oxygen flow drops, triggering an alarm.

Front line diary
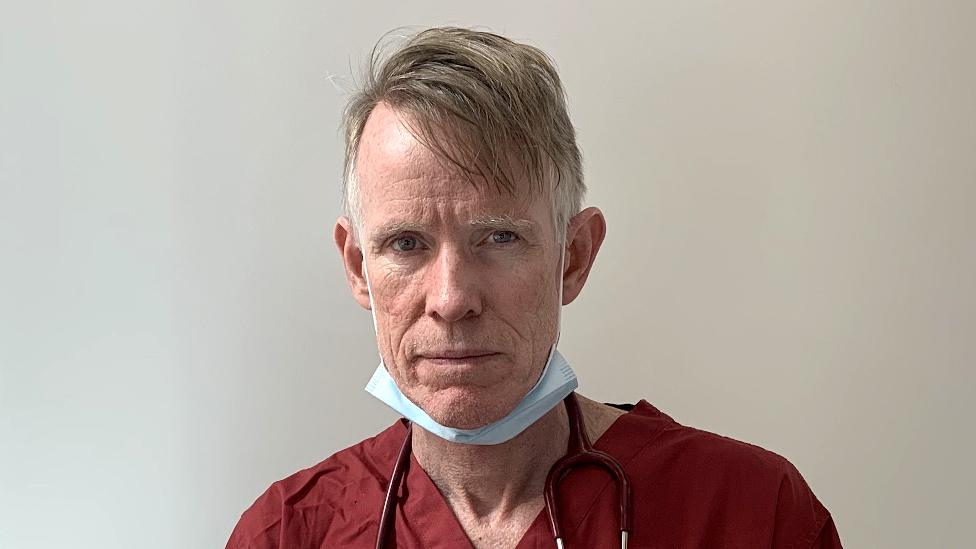
Prof John Wright, a medical doctor and epidemiologist, is head of the Bradford Institute for Health Research. He has looked after patients in epidemics all over the world, including cholera, HIV and ebola outbreaks in sub-Saharan Africa. Over the next few weeks he will be reporting for the BBC on how his hospital, the Bradford Royal Infirmary, is coping with Covid-19.
Read his first two diary entries: Why are people stealing hospital supplies? and Making life-and-death decisions

When we ordered extra equipment to deal with coronavirus cases, we were expecting the surge to come in May, but Covid-19 has turned out to be more transmissible than predicted and the peak is coming much sooner. So the extra ventilators aren't going to be here in time.
The form of non-invasive ventilation that appears to work best with Covid-19 patients is called Continuous Positive Airway Pressure (CPAP) but some of the hospital's CPAP machines use 50 litres of oxygen per minute for a single patient. This has never been a problem before, because oxygen is not usually in short supply. But in Italy it became a problem, because of the number of patients needing ventilation.

The army has been drafted in to deliver oxygen to hospitals
"One of the issues is that while beds have oxygen next to them, we've never needed such a large flow of oxygen on the ward," says Tom Lawton. "We have something like 250 litres per minute available for each ward, and about 3,000 available for the hospital - which again, has never been an issue before. But if you're using 50 litres per minute for each patient, then that's suddenly only five on a ward and 60 in a hospital - and we need more than that.
"It's not just us, it's also hospitals around the country - they weren't designed for this level of oxygen use."
Watford General Hospital declared a critical incident on Saturday as it neared the point when it would have been unable to provide oxygen to patients who needed it.

Listen to John Wright
John Wright is recording from the hospital wards for BBC Radio 4's NHS on the Front Line
You can hear the next episode at 11:00 on Tuesday 7 April, catch up with the first two episodes online, or download the podcast

Searching for ways round the problem, Tom has been working with Leeds University on a 3D-printed valve that could be attached to the hospital's ventilators to reduce the amount of oxygen they use.
But he also began looking at CPAP machines used to treat sleep apnoea at home. These maintain air at a continuous pressure, inside a mask, to keep the user's airways open - they have to be repurposed to provide oxygen for use in the hospital, but they use much less of it than standard hospital ventilators.
Tom called a local company to check availability.

Tom Lawton testing a continuous positive air pressure device usually used for sleep apnoea
"They said, 'Yes we've got 2,000, how many do you want?''' he says. "And so our plan is to start with 100 and to see whether, if we use these early enough during a patient's stay, we can prevent people deteriorating and needing to go on to the more complex ventilators, and needing to come to the intensive care unit."
We've been testing them over the weekend, and there's evidence from China and from the US that they seem effective. They just help inflate your lungs and that seems to be beneficial.
They are also very simple, which means that there's no need for a huge amount of training.

The first delivery of the simple CPAP machines
Debbie Horner, the consultant in charge of Covid-19 intensive care planning - who is now back at work after contracting the virus herself - says hospital doctors around the country took a sharp intake of breath when they heard that Italy was running out of oxygen.
"One of the issues that originally we didn't realise we were going to have is actually the diameter of the pipes coming into the hospital," she says. "So it's not just the total amount of oxygen that the hospital has, it's also how much can you get to the bedside? Or how many bedsides can you get oxygen to at any one time?"
We've had to consider how to distribute patients around the hospital "based on the size of the pipes", she says.
What everyone wants to avoid, through this kind of planning, is the situation that arose in Italy, where hospitals were unable to provide intensive care for all patients because of shortages of kit or staff.

3D-printed Venturi valves developed in Italy (left) and in Leeds (right) - the design will be posted on the internet
But a lot of thought is going into how we will deal with that situation if it arises.
"One of the things that we want to do in this hospital is to make sure that if we do reach that point, any individual clinician has support not only from other clinicians on the shop floor, but also from another group of senior doctors and clinicians within the hospital," Debbie Horner says.
"Beyond that, there's also discussion about regional and national ethics committees, to support the individual hospitals with that decision-making process, so that everybody is making those decisions using the same framework."
This is uncharted territory for us. There is a sense of dread about potentially having to replicate some of the decisions that have been taken in Italy.
Hopefully it won't reach that point.
Follow @docjohnwright, external on Twitter

A SIMPLE GUIDE: How do I protect myself?
AVOIDING CONTACT: The rules on self-isolation and exercise
LOOK-UP TOOL: Check cases in your area
MAPS AND CHARTS: Visual guide to the outbreak
