‘I was desperate for a cancer manual – but there isn’t one’
- Published
- comments
When James* found out his wife had been diagnosed with advanced cancer he began searching for a checklist of what he was meant to do. Here, he describes what it's like to discover there isn't one.
Cancer is an indiscriminate assassin, they say.
But when its presence is confirmed, it certainly doesn't seem that way.
It feels all too personal when everything comes crashing to the ground.
Even with two months' hindsight it is truly impossible to adequately describe the emotions in my head when the consultant said: "I'm very sorry, Ellen, it is Stage Four. It started in your bowel and has spread to your liver. There is no cure."
It felt like I was a second-rate actor in a daytime soap opera: failing to remember my lines, not knowing where to stand or what to do, despite the countless rehearsals that I'd performed in my mind in recent weeks as Ellen's discomfort grew along with her distended belly.
I can't even begin to imagine what it must have been like for my wife - a fit, strong and energetic 46-year-old with a zest for life and a passion for helping people - but I know my immediate desire was to swap places with her.
The consultant gently warned us before the diagnosis day appointment that Ellen may have to be admitted into an acute ward straight after the tests. He advised her to pack the 21st century equivalent of pyjamas and toothbrush: your phone, tablet and chargers.
He tried to go through the CT scan results as honestly, candidly and sensitively as possible.
But when you're in that situation all you want to hear are the answers to four questions: How bad is it? Will it kill Ellen? What treatments are there? And how long are we talking about?
Everything associated with cancer, we were quickly discovering, happens either at breakneck speed or with glacial slowness.
I'm sure he did it as quickly as he possibly could, and my perceptions of time were completely distorted by the sense of sheer terror, but it seemed like an eternity before he finally produced answers to questions one and two.
We would have to wait even longer for responses to questions three and four.
Everything associated with cancer, we were quickly discovering, happens either at breakneck speed or with glacial slowness.
While I was a gibbering mess, Ellen was stunned into a weird, calm silence. Her beautiful big brown eyes - the first thing I ever noticed about her when we met 17 years ago - struggled to take in the enormity of it all.
We gained a small crumb of comfort from the consultant pointing out that while Ellen's cancer had probably been cooking for at least a year, she had only been symptomatic for two to three months.
So there's nothing she or anybody else could have done differently.
Ellen acknowledges she was "in denial" during the first couple of months of feeling lethargic and rapidly losing weight.
But we both simply turned to a far more logical explanation: stress and anxiety caused by us both having demanding careers; working from home since mid-March due to the Covid-19 lockdown; and supporting our then 10-year-old son Joe's education while his school was closed.

Where do you turn?
During the first few days and hours after Ellen's diagnosis, I was desperate for a manual, a checklist, a guide on what the hell to do.
But there isn't one.
I know from more than 20 years in journalism, though, that one of the first things you do when you come across a new subject is to quickly consult as many experts as possible.
And so I messaged three friends and former colleagues who had lost their partners to cancer.
One of them is Steve Bland, who runs the award-winning and ground breaking You, Me and the Big C podcast which was co-created by his late wife and former BBC Radio 5 live presenter Rachael Bland.
The two years that have passed since her death have given Steve so much wisdom and a perspective he has kindly shared with me.
From the start, he reassured me there were no such things as weird or inappropriate thoughts and that it was entirely normal for me to be thinking: "I'm 44 years old - you can't be widowed that young. Will I ever meet anybody after my wife has gone, and how on earth could she ever compete?"
It's normal for your mind to race ahead, he said. It's how we humans try to make sense out of a senseless situation.

Other friends have urged Ellen and I to maximise every second, to live in the moment.
For me at least, that's far easier said than done.
You know how New Year's Eve is always hyped as a brilliant night out but all too often falls horribly flat because you're under so much pressure to have fun?
That's how it feels at the moment: nothing kills the mood more than knowing you're supposed to be having a great time.
And the clock is ticking in my head.
Even when we are enjoying some of life's simple pleasures - a leisurely lunch, a trip to the cinema - a voice pops up, whispering: "Don't be having too much fun: you know it won't last forever."
To borrow from that awful 2020 mantra, though, I am really trying to train my brain to cope with the new abnormal.

Breaking the news
I found sharing the news of my wife's diagnosis with friends and family traumatising, exhausting and almost all-consuming. You quickly forget who knows what, and feel guilty when you realise some friends have only heard via the grapevine.
Ellen suggested I create a Whatsapp group, so we'd only have to post updates once.
At first I thought it sounded horribly cold and impersonal, but in hindsight it's something I'd definitely recommend to anybody in a similar situation.
The coronavirus pandemic has seeped into so many aspects of our lives - none more so than when all you need is a hug from your mates.
When hearing and seeing a friend in distress, it's the most natural thing in the world to put your arms around them.
But when I told one - out in her front garden - neither of us knew what to do for a few seconds, until she told me to not be so stupid and to come inside immediately. I then just sobbed into her shoulder as she held me like a baby.
The hardest person to inform was our sweet and innocent yet worldly and wise son Joe.
How do you even begin to contemplate telling your child that his mum is going to die before he becomes a man?
We asked charities including Macmillan and our local Maggie's Centre, which provides a one-stop shop advice and support service for cancer patients and their families.
"Just tell him the truth as clearly as you can," we were advised. "Don't be afraid to say you don't know the answers to many of his questions, and don't be scared to cry."
At a time when it felt like we had precious little say over anything in our lives, we at least had total control over where, when and how we would drop the bombshell.
Certainly not at the hospital, and not until we'd tried to come to terms with it ourselves.
We chose straight after school on a Friday - so as to maximise the time before school again - and in the haven of our living room.
Joe's reaction was pretty much the same as mine: stunned, angry, disbelieving, sorrowful, confused.
We probably shouldn't have been surprised when he asked exactly the same four questions as I had.
"What treatment is there?" and "When will you die, mum? Will you see me become a teenager? What about starting high school next September?"

What impact has Covid-19 had?
Because our local GP surgery has for months been physically closed to patients due to Covid-19 precautions, all appointments have been carried out over the phone. They don't even have video-conferencing as an option.
This meant nobody saw Ellen in the flesh - and how emaciated she was - until diagnosis day.
While in her case the lack of face-to-face appointments probably didn't make a difference, what about the thousands of others who are going through similar ordeals?
Ellen's initial appointment at our local hospital was made even more difficult because initially I wasn't allowed to accompany her into the clinic.
Thankfully a kind-hearted security guard took one look at the pair of us before waving us in with his eyes.

When Ellen was subsequently admitted into the hospital's Covid sterile bubble, I was permitted a one-hour visit per day, and this was only granted because of how gravely ill she was.
At the weekend, I obtained permission from the ward manager to bring Joe in with me. The message never reached the security desk though and I was curtly asked: "What are you doing, bringing a child in with you?"
At this point Joe did not know the diagnosis and so I had to compose a text message on my phone, saying: "My wife has just been diagnosed as terminally ill. Our son here does not know, so please for heaven's sake do not say anything. We have permission to enter the acute ward while wearing masks. Please let us in!"
And apart from the initial consultation at the specialist cancer unit, I've not been allowed to accompany Ellen for any of her appointments, including chemo. This is unlikely to change in the months to come.
Having to drop your wife outside the main entrance - I think they're called "kiss and fly" zones at airports - in such circumstances is just awful, there's no other way of describing it.

Things I had no idea about
Cancer brings with it a whole new lexicon and layers of bureaucracy.
Starting with wills. Foolishly, Ellen and I assumed we didn't need one, given that we're a boring married couple. But it turns out that you do, especially if you have children.
And writing a will is much better done when you don't have a ticking clock for musical accompaniment.
We ended up drafting it in the back garden of a solicitor's house (so that we could be socially distanced in these crazy, messed up times).
"Have you thought about burial or cremation, Ellen?", he asked. "What about your wake, or having a massive party before you're gone? A friend of mine wants his ashes to be included in a big firework and be blasted into the atmosphere as Bat Out Of Hell blasts out."
It was almost unbearable for Ellen to listen to. While we all know the grim reaper will come knocking one day, hearing the words "after you die" is unbearable.
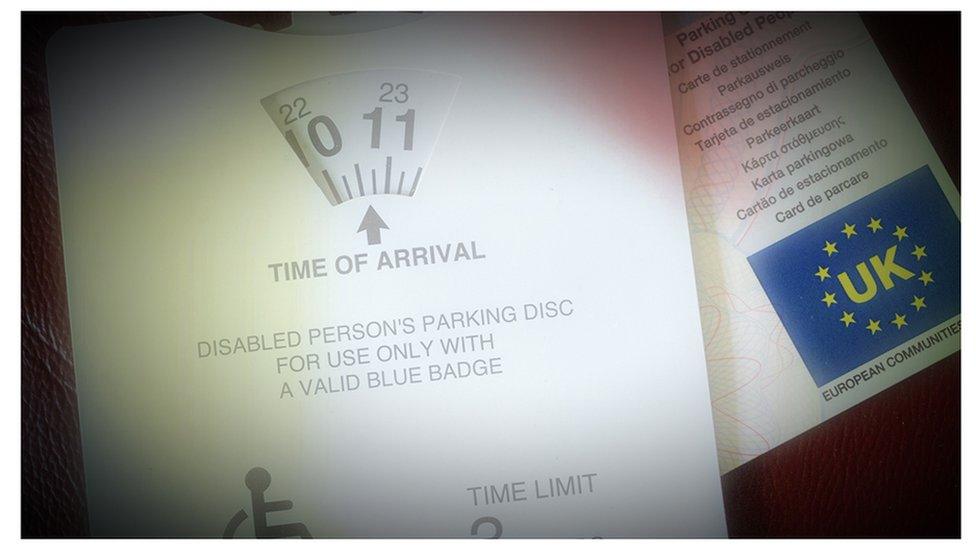
After the wills came the quest for the innocuous-sounding DS-1500 form which, at least in theory, is meant to see you glide through the alphabet soup of the benefits system: PIPs, DLAs, UCs.
To get the form, you need your doctor to certify that, in lay speak, they wouldn't be surprised if you kicked the bucket within six months.
While it was another sobering moment when the form came through, we cracked jokes that it was highly unlikely that somebody from the dole office would arrive after the allotted 26 weeks, carrying a clipboard and telling her that time was up.
We tried not to think too much about it, other than to welcome the news Ellen would get the Blue Badge she needs.
Honestly, until you're in the situation where either you or a loved one can't walk very far, you will have no idea how hard it can be to navigate your way around daily life.
My advice on all of the above is to seek advice - there are plenty of lovely and skilled people out there waiting to help.
For example, a benefits adviser at Maggie's was able to sort out the paperwork needed to obtain that Blue Badge, as well as to complete the myriad forms needed to obtain a Personal Independence Payment.
Having somebody skilled and well-versed with the system meant Ellen and I could try to focus on more pressing matters… and try to enjoy ourselves a bit.

The future
Keep kicking the can down the road because you never know what new treatments will be discovered.
Ellen has always been the organised one in our relationship, and has immediately started compiling two collections - a bucket list and one that rhymes with bucket.
And while we don't know how long we've got together - so much depends on how her treatment goes - we're hoping for at least a few good days each cycle in which more treasured memories can be made.
Days in which you live as opposed to merely existing. And live in the moment.
There is a phrase used by some cancer patients: keep kicking the can down the road because you never know what new treatments will be discovered.
Ellen is doing more than her level best on that front: the chemo is going remarkably well and she's also just started a form of relatively new immunotherapy that could, in her words, "double my expiry date".
She is determined not to be seen as a victim, and I'm reminded of something she said to me a day or so after being diagnosed.
"I'm not done yet, you know. Far from it."
With one eye on the future, though, I've asked Ellen to record herself leaving messages for Joe and me to play endlessly when she's no longer physically with us.
We're the first generation blessed with the technology to record and keep plentiful audio and video recordings of our loved ones.

Sadly the other most primeval sense cannot yet be captured: smell.
The pheromones that forever bond lovers, families, and fleeting, happy days.
In my mind's nose, I can recall every note of my nana's house. A heady mix of home-made apple pie, furniture polish, and cigarettes.
With Ellen, though, it's far harder, no impossible, to describe the constituent aromas. But I know how good it is, and how I cannot imagine not having it there any more. When she was in hospital those five nights, I went to sleep holding the pillow that she rests her head on, breathing her in.
And while my memories will never fade, I know the lingering odour on her clothes will slip out of my mental grasp.
Does anybody have a machine that can extract the very essence of Ellen please? I'd happily pay out thousands.
But for now, I'll enjoy the real thing.
*Names have been changed
Related topics
- Published16 December 2020

- Published6 September 2018

- Published6 September 2018

- Published15 January 2020
