Covid: Is there a limit to how much worse variants can get?
- Published

Oxygen cylinders in India, where the more transmissible Delta variant was first seen
It is clear we are now dealing with a virus that spreads far more easily - probably more than twice as easily - as the version that emerged in Wuhan at the end of 2019.
The Alpha variant, first identified in Kent, UK, performed a large jump in its ability to transmit. Now Delta, seen first in India, leapt further still.
This is evolution in action.
So are we doomed to a never-ending parade of new and improved variants that get harder and harder to contain? Or is there a limit to how much worse coronavirus can become?
It's worth remembering the journey this virus is on. It has made the jump from infecting a completely different species - its closest relatives are in bats, external - to us. It's like you, starting a new job: you're competent, but not the finished article. The first variant was good enough to start a devastating pandemic, but now it's learning on the job.
When viruses jump to humans it would be "very rare for them to be perfect," said Prof Wendy Barclay, a virologist from Imperial College London. "They settle in and then they have a great time."
There are examples of viruses, she said, from flu pandemics to Ebola outbreaks, making the jump and then accelerating.
So how far could it go?
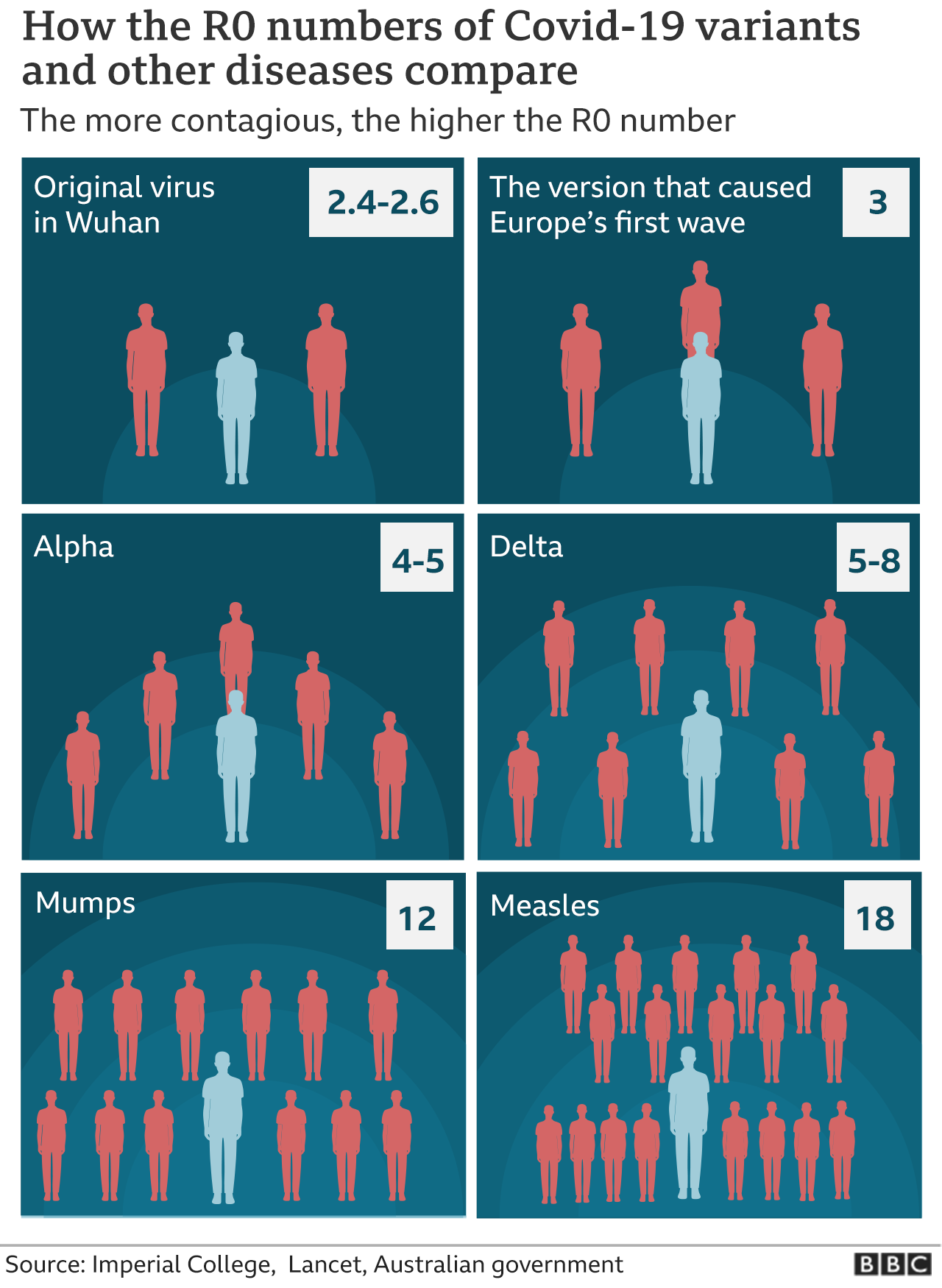
The cleanest way of comparing the pure biological spreading power of viruses is to look at their R0 (pronounced R-naught). It's the average number of people each infected person passes a virus on to if nobody were immune and nobody took extra precautions to avoid getting infected.
That number was around 2.5 when the pandemic started in Wuhan and could be as high as 8.0 for the Delta variant, according to disease modellers at Imperial.

"This virus has surprised us a lot. It is beyond anything we feared," said Dr Aris Katzourakis, who studies viral evolution at the University of Oxford. "The fact it has happened twice in 18 months, two lineages (Alpha and then Delta) each 50% more transmissible is a phenomenal amount of change."
It's "foolish", he thinks, to attempt to put a number on how high it could go, but he can easily see further jumps in transmission over the next couple of years. Other viruses have far higher R0s and the record holder, measles, can cause explosive outbreaks.
"There is still space for it to move higher," said Prof Barclay. "Measles is between 14 and 30 depending on who you ask, I don't know how it's going to play out."
So, how are the variants doing it?
There are many tricks the virus could employ to get better at spreading, such as:
improving how it opens the doorway to our body's cells
surviving longer in the air
increasing the viral load so patients breathe or cough out more viruses
changing when in the course of an infection it spreads to another person
One way the Alpha variant became more transmissible, external was by getting better at sneaking past the intruder alarm - called the interferon response - inside our body's cells. But this does not mean that by the time we work through the Greek alphabet of variants and reach Omega that we'll end up with an unstoppable beast.
"Ultimately there are limits and there isn't a super-ultimate virus that has every bad combination of mutations," said Dr Katzourakis.

There is also the concept of evolutionary trade-offs - in order to become better at one thing you often get worse at something else. The fastest vaccination programme in history will give the virus a different hurdle to overcome and squeeze it in another evolutionary direction.
"It is quite possible that changes in the virus that make it better at avoiding vaccines could end up compromising its ability to transmit in an absolute sense," said Dr Katzourakis.
He thinks the Beta variant - which has a mutation called E484K that helps evade the immune system but hasn't managed to take off - is an example of this. However, the Delta does have mutations that both help it spread and partially dodge immunity.
What will turn out to be the optimal strategy for coronavirus is still hard to predict. Different viruses use different techniques to keep on infecting. Measles is explosive, but leaves behind lifelong immunity so it always has to find someone new. Influenza has a much lower R0, barely above 1, but constantly mutates to side-step immunity.
"We're in a really interesting, intermediate and somewhat unpredictable phase, it is difficult to predict how that's going to play out a year from now," said Prof Barclay.
One thing that is often claimed, but attracts scientific scorn, is that the virus must get milder in order to spread more easily. There is very little evolutionary pressure on the virus for that to happen. The virus is already off into the next person long before it kills the person it infected. And the people who do the most spreading (younger people) are those who don't get very ill.
In rich countries with good vaccination campaigns it is hoped the next variants won't be able to pose a major problem due to widespread immunity. But these progressively more transmissible variants are a nightmare for the rest of the world where they are making it harder and harder to stay on top of Covid.

VACCINE PLEDGES: How many have US and others promised?

Follow James on Twitter, external