'A&E is absolute chaos - I spent 15 hours on a trolley'
- Published

Anne Whitfield-Ray said that despite her experience she cannot fault NHS staff: "They are doing the best they can"
Lying on a trolley in a hospital corridor in pain from a broken hip, Anne Whitfield-Ray could not believe she was in the care of the NHS.
"It was absolute chaos - like something out of a third world country," said the 77-year-old from Worcestershire.
"The staff were rushed off their feet, paint was peeling off the walls and patients were being squeezed in everywhere they could - in makeshift bays, in corridors and side rooms. It was horrific."
Anne spent 15 hours in that position until a bed could be found for her.
Such delays used to be the exception, something that happened on the odd occasion in the depths of winter.
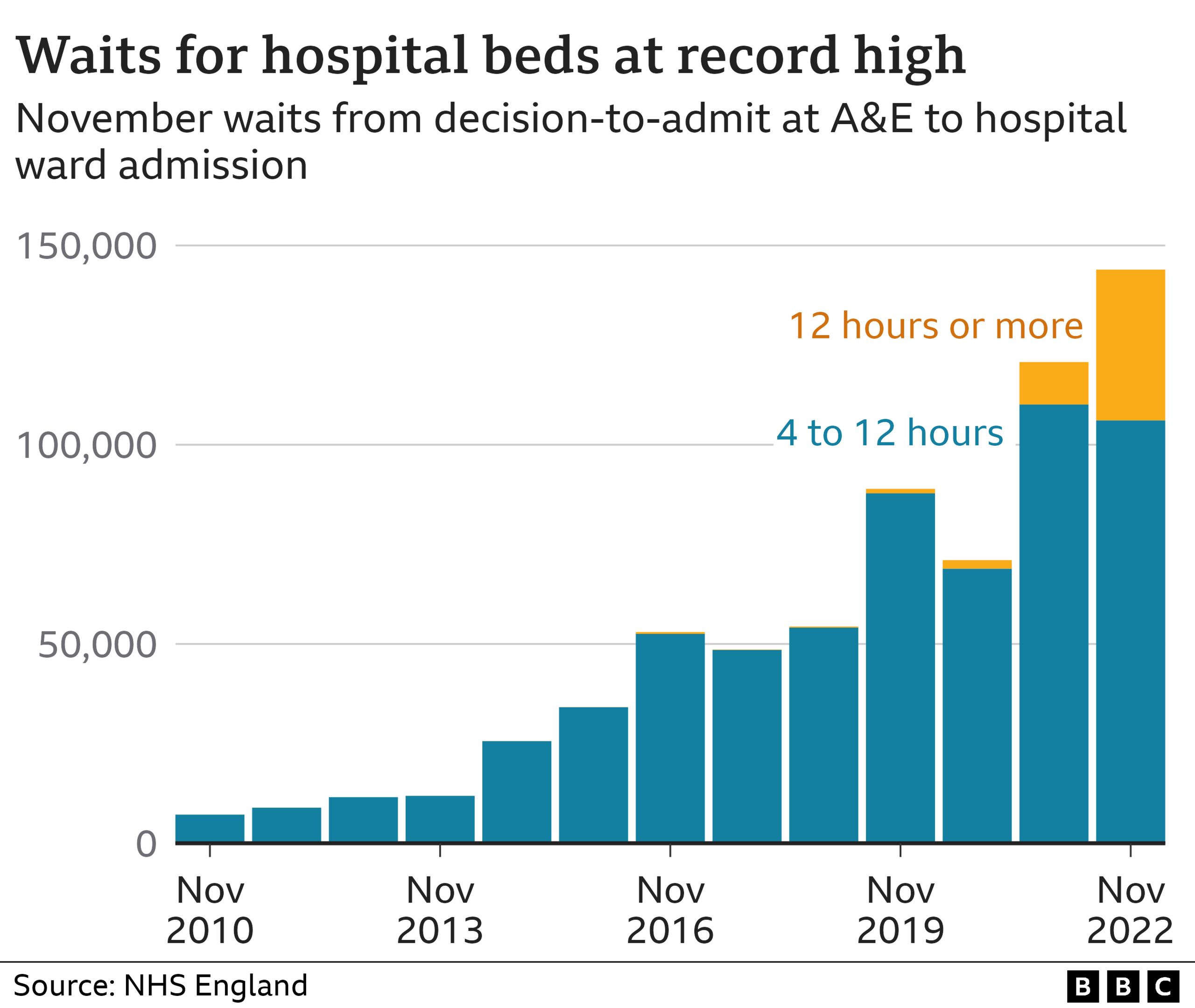
Now they are commonplace. Latest figures show nearly 40% of A&E patients who need admitting face what is called a trolley wait - a delay of four hours or more waiting for a bed to be found.
Around 10% are waiting over 12 hours. To put that in context, there have been more 12-hour trolley waits in 2022 so far than in the past 10 years combined. Similar pressures are being reported in other parts of the UK.
These are the sickest and frailest patients - the ones who cannot be sent home immediately after treatment. Research has linked delays like this with longer hospital stays and even a higher risk of death.
By the time patients get to this point, they may have already faced hours of waiting in A&E or, increasingly, stuck outside A&E in the back of an ambulance, as was the case for Anne.
She is now back home recovering after surgery, a few days after her fall in October.
She said that despite her experience she cannot fault the staff: "They are doing the best they can. But this is not what should be happening in the NHS.
"There are people much worse off than me - people who have strokes and heart attacks and face delays too."

Dr Adrian Boyle, of the Royal College of Emergency Medicine, said it is the plight of patients like Anne that worries him the most.
"We are not doing the right thing by patients. There are lots of risks to people spending these long stays in emergency departments. Their care is delayed and diluted.
"Elderly people become delirious - it's a miserable experience for them. And I see people regularly who are just so tired that they become confused, and it doesn't help them get better."
Dr Boyle said that once someone has spent more than six hours in A&E, there is a real increase in the risk of severe harm: "We really need to stop people having these long stays in emergency departments."
'Fundamental challenge'
Dr Vin Diwakar, of NHS England, said staff were working "round-the-clock" to try to see and treat patients as quickly as they can.
He said the problems in A&E were caused by a lack of beds, with 19 out of every 20 currently occupied.
He said the "fundamental challenge" was the difficulty hospitals were facing discharging patients who were medically fit to leave, but could not be released because of a lack of care in the community.
Every day more than half of patients ready to be discharged cannot be discharged.
Dr Diwakar said steps were being taken, including investment in community teams to stop people ending up in hospital,
A network of regional "war rooms" has also been created, he added, which monitor the pressures on local hospitals in real time, so they can try to manage demand by diverting ambulances away from the most under-pressure hospitals.
Additional reporting by Kris Bramwell.
- Published21 October 2022

- Published18 October 2022

- Published24 November 2022
