The NHS backlog: Who are the 7 million?
- Published

There are more than seven million people on a hospital waiting list in England - one in eight of the nation's entire population.
Many have spent months waiting to be seen.
But who are these people and what is the impact on their lives? The BBC has been investigating the backlog to find out.
'All-consuming pain'
Jane Probyn has spent much of the past three years on an NHS waiting list. She has osteoarthritis and was referred for a hip operation in October 2020.
Before surgery could be completed, however, came the fallout from the Covid pandemic, meaning nearly all routine hospital treatment was stopped. It was March 2022 by the time Jane had her right hip replaced.
By that point, her left hip had deteriorated so badly that it needed replacing too. She is still waiting for that operation.

Jane Probyn has been on an NHS waiting list for more than two years
"I am in constant pain," says the 66-year-old, from Cambridge. "It's all-consuming and is overshadowing every aspect of my life.
"I can't walk properly and have to rely on a walker and mobility scooter to get around.
"I can't look after my grandchildren. It is spoiling my retirement.
"The most frustrating thing is not really knowing when I will get treated. My life is on hold."
Knees, hips, eyes - what tops the waiting list?
Jane is not alone. Nearly 800,000 people require hip, knee and joint-related orthopaedic treatments. Close to half of them have been waiting longer than 18 weeks, which is not just the target waiting time but supposedly a patient right, written into the NHS Constitution.
Deborah Alsina, chief executive of the charity Versus Arthritis, says these long delays are having a "devastating" effect, both physically and mentally, as many of the patients her charity supports end up clinically depressed.
Among the waiting backlog are a broad range of patients needing a wide variety of care.
There are 640,000 waiting to see eye specialists - many will have declining eyesight with its obvious consequences on their daily lives - and there are more than 500,000 waiting for gynaecological care and another 500,000 waiting for ear, nose and throat (ENT) treatments.
Not all of them will need to have an operation: fewer than a quarter of patients on the waiting list end up undergoing surgery - with medication and care, such as physiotherapy, more common when patients are finally diagnosed.

Nonetheless, Prof Neil Mortensen, president of the Royal College of Surgeons of England, says the situation has left his members feeling they are letting down patients. "Their health may be worsening by the day; their independence being slowly eroded and quality of life deteriorating while they wait."
'Heart disease can't wait'
The backlog is often referred to as a waiting list for routine, or non-urgent, treatment. But it does include more than 300,000 people with heart-related problems - a third of whom, currently, have waited more than 18 weeks.
Some are waiting for tests, such as CT scans and echocardiograms, or procedures - such as stents and balloons to open blocked arteries, as well as pacemakers. Others need heart surgery, such as transplants or a bypass.

Garry Cogan is one of more than 300,000 people waiting for heart-related treatment
Garry Cogan, 62, from Essex, is one of them. He needs a triple heart bypass after having a heart attack last year. He hopes to undergo surgery early next year, but says the wait has been agonising.
"I'm constantly living in fear, worried I could have another heart attack at any point. I can't go on holiday and have had to cut back how many days I work, which is difficult financially."
British Heart Foundation associate medical director Dr Sonya Babu-Narayan says the delays are a real risk for patients like Garry. "Tragically, we've already seen tens of thousands of extra deaths involving heart disease since the pandemic began - and disruption to heart care has likely contributed.
"We can't afford to let long waits for heart care become the status quo because heart disease can't wait. Delays can result in avoidable heart failure, or even death."
There will also be thousands of yet-to-be diagnosed cancer cases. Around a fifth of cancer cases are diagnosed through routine referrals where the disease is not suspected by a GP, but subsequent tests given while patients are on the general waiting list reveals cancer is present.
An analysis by NHS data experts Insource has estimated there could be as many as 25,000 people on the waiting list with cancer, external who are not aware of it yet. The longer it takes to get through the backlog, the poorer their chances of survival will be.
Backlog causing children to miss school
Also on the list are more than 360,000 children. They are waiting for an assortment of treatment, from surgery for growth-related problems and major dental work through to tests for abdominal pain and breathing difficulties.
The numbers are rising all the time - in the past 18 months the overall number of children waiting has risen by 50%.
The Royal College of Paediatrics and Child Health is very worried about their plight. Dr Mike McKean says, in the worst cases, children are having to miss school: "We need to do something to protect children, young people and their families from lasting consequences."
But it is not just the fact the backlog is growing. The number of patients facing long waits is also rising, despite government efforts to address the issue.
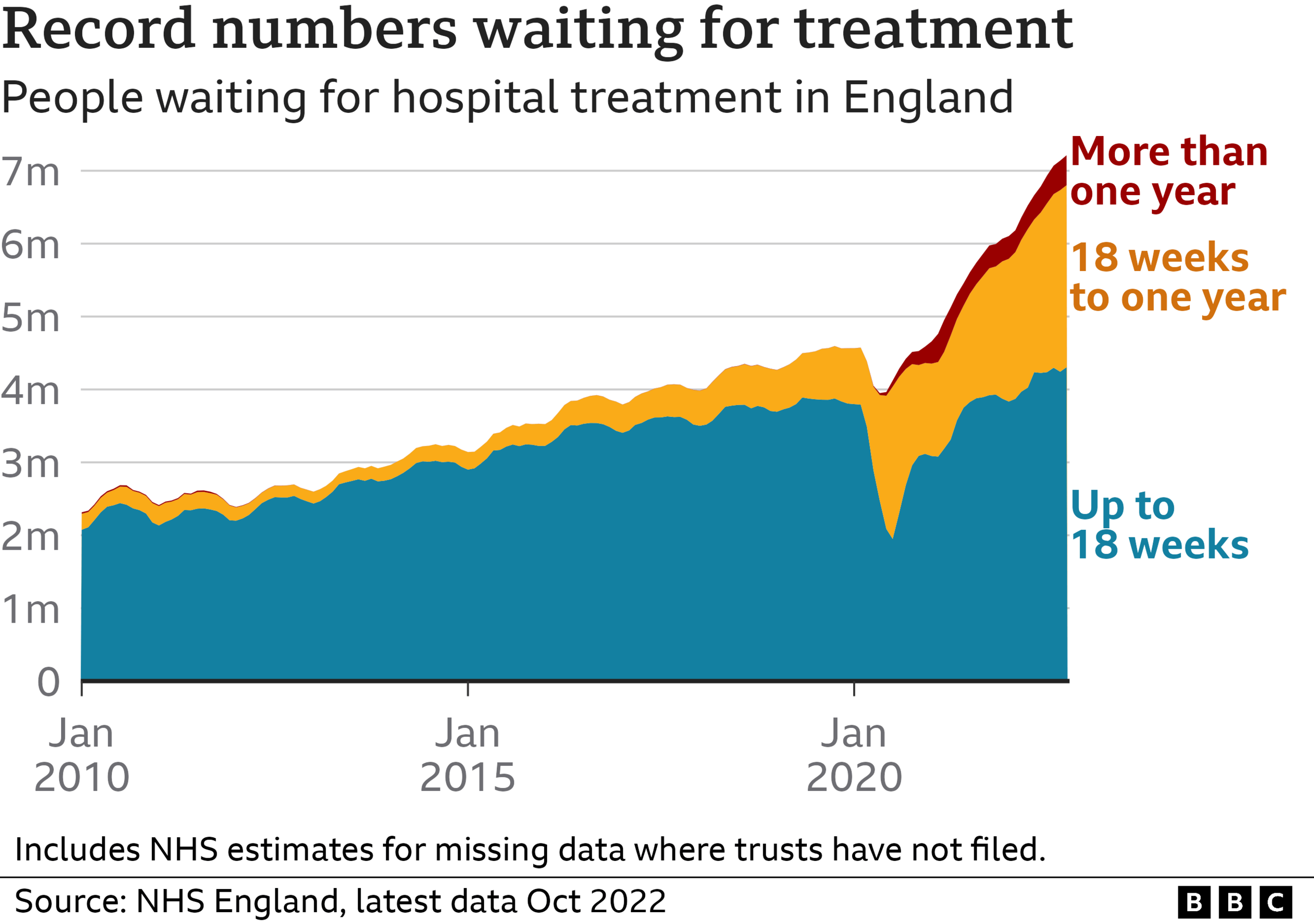
While the NHS has managed to eliminate two-year waits almost entirely, the number of patients who spend more than a year on hospital lists, such as Garry, is continuing to rise.
There are now more than 400,000, among the 7.2 million people waiting in England, in this position - a rise of a third over the past year. Before the pandemic, fewer than 2,000 patients were waiting more than a year.
The NHS's 18-week target now appears a distant dream. Currently 40% of patients have spent longer than that on waiting list.
But there is a huge variation between hospitals. Where you live in the country can make a big difference too.
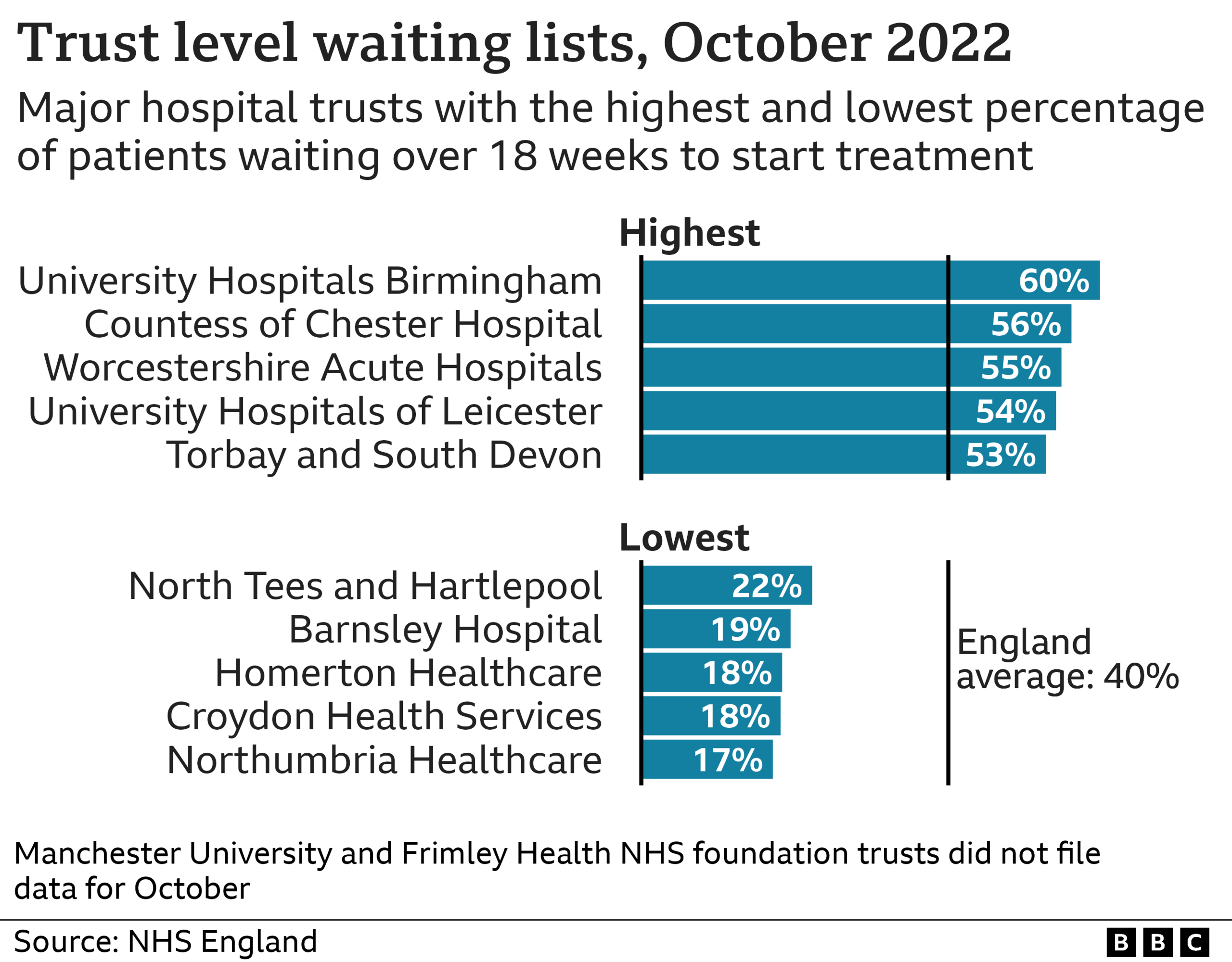
It is a similar story across the rest of the UK: in Scotland more than 25% are waiting longer than 18 weeks, in Wales - where there is a 26-week target instead of 18-week - nearly half of patients are waiting longer.
In Northern Ireland the situation is even worse - more than half of patients there have waited over a year.
Some patients giving up
Faced with such long waits, some patients are simply giving up. Those that can afford it pay to go private - a trend that appears to be becoming increasingly common.
But there are others that have dropped off the waiting list, and are left struggling with their health issues.
That is the case for Jane Nandi, from Nottingham. She has a non-cancerous lump on her tongue, known as a lymphatic malformation. It is the size of a small plum and prevents her eating foods which require a lot of chewing.
"If I catch it or bite it, it bleeds really easily," says the 56-year-old. "I can't eat an apple, or crisps, or foods like that."
Since the condition is not common, the treatment she needs is not available at every hospital. The service that was due to treat her informed her earlier this year they could no longer carry out the treatment.
She has not sought a referral elsewhere: "You just lose the fight.
"I'm just putting up with it for now and will maybe try again next year. Perhaps things will be a bit better then."
Data analysis by Christine Jeavans
Related topics
- Published5 July 2023

- Published5 July 2022

